Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Dental Journal
versão On-line ISSN 0375-1562
versão impressa ISSN 0011-8516
S. Afr. dent. j. vol.69 no.9 Johannesburg Out. 2014
CLINICAL REVIEW
HIV-associated salivary gland enlargement: a clinical review
S EbrahimI; B SinghII; SS RamklassIII
IF.C.S (S.A), M.Med (Surgery), M.S (Epidemiology); Departments of Surgery, Nelson R. Mandela School of Medicine, University of KwaZulu-Natal, South Africa
IIF.C.S.(S.A.), M.D.; Departments of Surgery, Nelson R. Mandela School of Medicine, University of KwaZulu-Natal, South Africa
IIIB. Physiotherapy M. Education, D. Education; Postgraduate research3, Nelson R. Mandela School of Medicine, University of KwaZulu-Natal, South Africa
SUMMARY
Salivary gland disease is well established as an important HIV associated oral lesion. It manifests as salivary gland swelling involving one or both parotid glands with or without xerostomia. In the context of HIV, the swelling may be due to a wide spectrum of pathological conditions that include reactive or inflammatory disorders, acute and chronic infections, and neoplasms. This paper reviews the epidemiology, pathogenesis, clinical presentation, aspects of diagnosis and management of HIV associated salivary gland enlargement, in particular parotid gland enlargement, due to benign lymphoepithelial cysts (BLEC). Parotid gland enlargement is typically an early manifestation in the HIV-positive patient and should alert healthcare professionals to the likelihood of HIV infection. FNAC of the parotid gland is required to confirm the diagnosis and instituting HAART forms an important part of the management. There is a shift away from surgery in the treatment of this essentially ‘benign’ condition.
Keywords: HIV, salivary gland disease, parotid enlargement, benign lymphoepithelial cysts
INTRODUCTION
Salivary gland disease is well established as an important Human Immunodeficiency Virus (HIV) associated oral lesion1 and salivary gland enlargement may be its initial clinical manifestation.2 The term HIV-associated salivary gland disease was first described by Schiodt et al as salivary gland swelling involving one or both parotid glands with or without xerostomia.3 These lesions may lead to considerable morbidity due to facial disfigurement, pain and discomfort.1,4 In the context of HIV, the swelling may be due to a wide spectrum of pathological conditions that include reactive or inflammatory disorders, acute and chronic infections, and neoplasms.2 This paper reviews the epidemiology, pathogenesis, clinical presentation, aspects of diagnosis, and management of HIV-associated salivary gland enlargement, in particular parotid gland enlargement, due to benign lymphoepithelial cysts (BLEC).
ACRONYMS
BLEC: benign lymphoepithelial cysts
BLEL: benign lymphoepithelial lesions
CT: computed tomography scanning
CMV: Cytomegalovirus
DILS: Diffuse infiltrative CD8 lymphocytosis syndrome
ELISA: Enzyme linked immunoassay
EBV: Epstein Barr Virus
FNAC: fine needle aspiration cytology
HAART: highly active antiretroviral therapy
KS: Kaposi's sarcoma
MRI: Magnetic resonance imaging
NHL: Non-Hodgkin's lymphoma
EPIDEMIOLOGY OF HIV ASSOCIATED SALIVARY GLAND DISEASE AND ENLARGEMENT
Head and neck lesions associated with HIV arise in over 50% of HIV- positive patients and occur in nearly 80% of all patients with AIDS.4,5 The average prevalence of HIV associated salivary gland disease in Africa was estimated to be 19%,6 with a study from Tanzania reporting prevalence to be as high as 47%.7 In other developing countries such as Thailand, the prevalence of HIV associated salivary gland disease is low at 1%.6 Prevalence of salivary gland enlargement in HIV-infected patients as reported from European and North America studies is about 1%-10%,8 with BLEC present in 3%-6% of these cases.4,9 In a recent South African study, 23.3% of patients were diagnosed with BLEC.10 Reasons for the high prevalence rates of HIV- associated salivary gland disease in Africa are unknown. It may be due to the presence of HLA-DR5 and untreated advanced stage AIDS in Africans.6 Malnutrition is rife in many African countries and this is an important factor in inducing oral mucosal disruptions, thus playing a role in the pathogenesis of HIV-associated salivary gland disease.11 However, direct comparisons of prevalence studies within Africa and Asia; and between developing and developed countries are at best speculative due to the small number of reports from developing countries, as well as differences in study design and data collection between studies.11
PATHOGENESIS
Parotid gland enlargement is commonly due to the development of BLEC within the parotid gland. To date, the precise aetiology of these lesions is unknown,12 and the pathogenesis has prompted much controversy.4 BLEC is defined as single or multiple cysts within lymph nodes situated mainly along the tail of the parotid gland that have been trapped during parotid gland embryogenesis. It is therefore not surprising that it is this region of the parotid gland that enlarges early on during the course of the disease process. This lymphoid proliferation may result in ductal obstruction and ductal dilatation that mimics a true cyst. Parotid enlargement may also result from proliferation of the glandular epithelium that is trapped within these intra-parotid lymph nodes. HIV has a predilection for lymphoid tissue and elevated concentrations of the virus can be found within these nodes.4,12,13
In a subgroup of HIV-positive patients, a disease process known as "Diffuse infiltrative CD8 lymphocytosis syndrome" has been observed. This entity is characterized by a CD8 lymphocytosis, bilateral parotid swelling, a diffuse visceral CD8 lymphocytic infiltration (usually involving the lung), and cervical lymphaden-opathy.14 An immunogenetically distinctive group (HLA- DR5) is particularly predisposed to this pathology.15
There is considerable debate as to the terminology used to describe these lesions. The terms include benign lymphoepithelial cysts (BLEC), benign lymphoepithelial lesions (BLEL), cystic BLEL, AIDS-related lymphadenopathy, diffuse infiltrative CD8 lymphocytosis syndrome (DILS), cystic lymphoid hyperplasia and HIV associated salivary gland disease.4
CLINICAL PRESENTATION
Among the salivary glands that may be affected by HIV infection, the parotid is most widely involved. Exceptionally, the submandibular gland may be affected.16 In a South African study, the parotid gland was implicated in 35.4 % of patients, whilst submandibular involvement was recorded in 10.1% of patients.10 BLEC of the parotid gland usually present as painless bilateral parotid enlargement,17 although unilateral parotid swelling has also been documented.4 This is accompanied by diffuse cervical lymphadenopathy.18 Typically the patients may be very well without suspicion or concern for immunodeficiency, the clinical presentation being prompted by cosmesis. The cysts can enlarge, or cause discomfort, in addition to being cosmetically unacceptable to patients.19 The association between BLEC and HIV is usually during the early phases of viral infection, but it can affect patients at any stage of HIV.20,21
The clinical assessment of patients with HIV and parotid swelling involves taking a thorough history related to the time of onset and rate of growth as well as symptoms associated with the mass such as pain and discomfort. Constitutional symptoms such as fever, loss of weight and night sweats should alert the practitioner to the possibility of TB or lymphoma; a sudden increase in gland size should arouse suspicion of possible lymphomatous transformation. On physical examination, both parotid glands must be investigated for masses and the neck for lymphadenopathy. Features of malignant transformation such as induration, pain, fixation and facial nerve pathology should also be noted.22
The differential diagnosis of BLEC includes branchial cysts, salivary duct cysts, reactive lymphadenopathy, traumatic sialocoeles, Sjogren's syndrome, lymphangiomas, tuberculous abscesses, cystic tumours, malignancies (for example cystadenocarcinoma), as well as those due to Non-Hodgkin's lymphoma (NHL) and Kaposi's sarcoma (KS).10,19 These conditions are important to consider and exclude using the diagnostic methods described below.
ASPECTS OF DIAGNOSIS
The diagnosis of BLEC is very specific to HIV infection. Thus, if confirmed in a patient with an unknown HIV status, it is mandatory to perform an HIV test as part of the diagnostic work- up.23
Diagnostic modalities may be non-invasive and invasive. Non-invasive diagnostic evaluation consists of an ultrasound scan of the parotid gland, computed tomography scanning (CT) and/or magnetic resonance imaging (MRI) in cases of diagnostic ambiguity. Ultrasonography is ideal for evaluating "superficially located anatomic soft tissue entities" such as the parotid gland.9 Furthermore, its advantages include that it is easy to perform, painless, inexpensive, readily available and obviates radiation exposure to patients.9 Additionally, ultrasonography allows for evaluation of both cystic and lymphoproliferative lesions of the parotid glands. In a study by Kabenge et al (2010), four distinctive ultrasound patterns in the parotid glands of HIV-positive patients were described. These include: lymphocytic aggregations, lymphoepithelial cysts (prominent round hypo-echoic areas with well circumscribed margins and internal septa), fatty infiltration (in patients on protease inhibitor therapy) and lymphadenopathy.24 Typical CT scan findings are single or multiple bilateral parotid cystic lesions or densely enlarged parotid glands suggestive of massive CD8 infiltration.13
Invasive procedures include fine needle aspiration cytology (FNAC) of the parotid gland, which is a safe and suitable diagnostic modality and is recommended to exclude the lesions that may be considered in the differential diagnosis.23 It is also important to exclude malignancy which may occur in a small percentage (<1%) of patients with HIV associated cystic lesions and in solid lesions where the incidence of malignancy can be as high as 40%.25 Aspiration of BLEC typically reveals yellow mucous type fluid. Fine needle aspiration cytology of BLEC reveals a heterogeneous lymphoid population, scattered foamy macrophages and anucleated squamous cells in a proteinaceous background.10,22
The diagnostic criteria for DILS comprises HIV seropositivity as confirmed on enzyme linked immunoassay (ELISA) and Western Blot testing, bilateral salivary gland enlargement, or xerostomia persistent for more than six months and histologic confirmation of a salivary or lacrimal gland granulomatous inflammation or a neoplastic involvement.26 There is a consistent CD8+ lymphocytic infiltration on minor salivary gland biopsy.22 Other histopathological features range from complete preservation of glandular structures, to considerable distortion of the normal glandular architecture and fibrotic changes.27 It is worthwhile to note that patients who are diagnosed with DILS have a four-fold risk of developing NHL.28
The aetiology of BLEC remains obscure. The role of epidermotropic viruses such as Epstein Barr Virus (EBV) and Cytomegalovirus (CMV) has been suggested. However conflicting reports exist in the literature as to the main causative organism.29 Further studies using immunohistochemistry and in situ hybridization techniques are necessary to elucidate the role of EBV and CMV in the pathogenesis of BLEC.29
In summary, the main diagnostic modalities for BLEC include ultrasonography and FNAC of the parotid gland. The key diagnostic features for HIV-associated BLEC described by Meyer et al,30 include: manifesting in the chronic or latent phase of HIV disease, cysts (often bilateral and multiple) with associated cervical lymphadenopathy, ultrasonography demonstrating multiloculated, large bilateral thin-walled preparotid or parotid cysts; dense nodular infiltrate in and around the parotid gland with cervical lymphadenopathy and FNAC results showing a clear, proteinaceous fluid with epithelial and lymphoid cells.
MANAGEMENT OF HIV- ASSOCIATED PAROTID GLAND ENLARGEMENT
The management of parotid gland BLEC is controversial with different opinions as regards the best treatment option.4 Management choices include a wholly conservative approach involving serial follow-up and observation of lesions, aspiration of lesions, sclerosing therapy, highly active antiretroviral therapy (HAART), radiation therapy, and surgery.4
For minimally symptomatic lesions without significant cosmetic deformity, monitoring is a viable option and should be at six-monthly intervals, with radiographic and histopathologic analysis undertaken where necessary to exclude malignancy. BLEC are slowly progressive lesions and any sudden increases in gland size requires prompt investigation due to the risk of lymphomatous transformation.4 Patients with DILS are susceptible to the development of NHL, and thus continued observation is mandatory. If there are no clinical manifestations of malignancy, monitoring of the patient together with an annual needle aspiration biopsy of the parotid gland to detect early malignant transformation represents a reasonable standard of care.13
Aspiration affords rapid relief, but cysts tend to recur within weeks to months and continue to enlarge.4 In addition, cysts may be multiple, loculated and of varying size, making complete aspiration difficult.12 Sclerotherapy with tetracycline and doxycycline4 as well as intralesional bleomycin19 and alcohol30 have been used with varying degrees of success. Cyst size reductions of between 42 to 100% have been reported.4
HAART has been shown to reduce the incidence of BLEC and DILS.4,22,31 Paradoxically, some studies show an overall increase in the prevalence of salivary gland pathology in the HAART era.32,33 Likely reasons to explain this phenomenon include the size of pre-existing lesions, duration of therapy, different HAART regimens34 and discrepancies in HAART availability in developing countries.35 Additionally, the initiation of HAART with subsequent lowering of HIV viral load and rise in CD4 counts may precipitate the activation of opportunistic infections that may have otherwise been clinically dormant (the so-called immune reconstitution syndrome) suggesting that an infectious agent may play a role in the etiology of HIV-associated salivary gland disease and enlargement.1,18 In contrast, significantly lower prevalence rates of DILS in the post-HAART era are reported, signifying that DILS is an antigen (viral)-driven response with the key treatment being antiretroviral therapy.36 HAART may also be combined with a short course of tapered-dose corti-costeroids in the treatment of these lesions.12 HAART has been successful in eradicating parotid swellings due to a cessation of viral replication, a decrease in viral load and stabilization of CD4/CD8 cell counts.37 Treatment is life-long because the immune system cannot clear residual virus.37 The possibility of HAART-induced lipodystrophy syndrome and deposition of fat in the paraparotid region is relevant. This disease process may clinically mimic parotidomegaly but is easily distinguished from true HIV-associated parotidomegaly on standard imaging modalities.14
Promising results have also been reported with the use of low-dose external beam radiotherapy (24Gy in 1.5Gy daily fractions).12 The reduction in size of BLEC lesions usually lasts less than ten months.22
Surgery for BLEC is challenging. For benign parotid pathology such as pleomorphic adenoma, either the superficial or deep lobe is removed; in BLEC, the entire parotid gland is affected, necessitating a total parotidectomy. The vascularity of the parotid gland, underlying sialadenitis and cystic changes that are part of the pathological process leads to distorted tissue planes, with displacement of the facial nerve, making dissection extremely hazardous. Thus, facial nerve injury, bleeding and seroma formation may occur.12 Since these patients usually present with a cosmetic problem there is little justification for an extensive operative procedure with its attendant morbidity. In view of the lack of Level 1 evidence to guide therapeutic options for HIV associated salivary gland enlargement, it is reasonable to embrace more conservative options. Surgery may be feasible in cases of poor response of parotid lesions to the treatment options listed above, or where there is concern that a lesion may have malignant potential.12
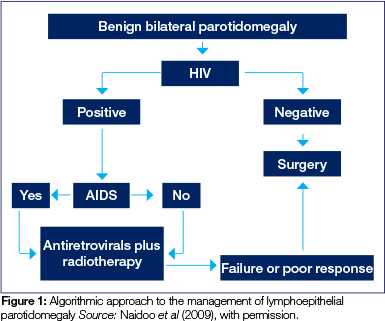
A useful management algorithm has been proposed by Naidoo et al (Figure 1).12
CONCLUSION
Oral lesions are important clinical Indicators of HIV Infection and may also point toward disease progression to AIDS.38 A better understanding of these orofacial complications is crucial due to the increasing worldwide burden of HIV disease, together with the fact that these lesions affect patients' quality of life,2,6 In a proportion of patients, HIV-associated salivary gland enlargement may be the initial manifestation of HIV infection, Thus, surgeons, together with other health care professionals, are uniquely placed in their current practices to make a significant impact on this disease entity, through timeous patient screening and referral for appropriate clinical care including HAART.39,40,41
There is a paucity of literature describing aspects of HIV-associated parotid gland enlargement especially from developing countries, including South Africa, In these areas, where HIV infection is rampant, and healthcare resources are limited, epidemiological studies and research on feasible diagnostic and management modalities are critical to reduce further morbidity.11
Conflict of Interest:
The authors declare no commercial or other association that might pose a conflict of interest with regard to this study.
Declaration:
No financial aid was sought or received to support this work.
This study was part of a thesis submission by Sumayyah Ebrahim (July, 2012) to the University of KwaZulu-Natal (UKZN) for the degree of Master of Medicine (Surgery).
References
1. Jeffers L, Webster-Cyriaque J. Viruses and Salivary Gland Disease (SGD) Lessons from HIV SGD. Advances in Dental Research. 2011;23(1):79-83. [ Links ]
2. Leao JC, Ribeiro C, Carvalho AAT, Frezzini C, Porter S. Oral complications of HIV disease. Clinics. 2009;64(5):459-70. [ Links ]
3. Schi0dt M, Dodd CL, Greenspan D, Daniels TE, Chernoff D, Hollander H, et al. Natural history of HIV-associated salivary gland disease. Oral surgery, Oral Medicine, Oral Pathology. 1992;74(3):326-31. [ Links ]
4. Shanti RM, Aziz SR. HIV-associated Salivary Gland Disease. Oral and Maxillofacial Surgery Clinics of North America. 2009;21(3):339-43. [ Links ]
5. Yengopal V, Naidoo S. Do oral lesions associated with HIV affect quality of life? Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics. 2008 7;106(1):66-73. [ Links ]
6. Ranganathan K, Hemalatha R. Oral lesions in HIV infection in developing countries: an overview. Advances in Dental Research. 2006;19(1):63-8. [ Links ]
7. Matee M, Scheutz F, Moshy J. Occurrence of oral lesions in relation to clinical and immunological status among HIV-infected adult Tanzanians. Oral Diseases. 2000;6(2):106-11. [ Links ]
8. Frezzini C, Leao JC, Porter S. Current trends of HIV disease of the mouth. Journal of Oral Pathology & Medicine. 2005;34(9):513-31. [ Links ]
9. Mandel L. Ultrasound findings in HIV-positive patients with parotid gland swellings. Journal of Oral and Maxillofacial Surgery. 2001;59(3):283-6. [ Links ]
10. Michelow P, Dezube BJ, Pantanowitz L. Fine needle aspiration of salivary gland masses in HIV-infected patients. Diagnostic cytopathology. 2012;40(8):684-90. [ Links ]
11. Holmes HK, Stephen LXG. Oral lesions of HIV infection in developing countries. Oral Diseases. 2002;8:40-3. [ Links ]
12. Naidoo M, Singh B, Ramdial P, Moodley J, Allopi L, Lester B. Lymphoepithelial lesions of the parotid gland in the HIV era-a South African experience. South African Journal of Surgery. 2009;45(4):136-41. [ Links ]
13. Mandel L, Surattanont F. Bilateral parotid swelling: a review. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics. 2002;93(3):221-37. [ Links ]
14. Mandel L. Salivary Gland Disorders. Dental Clinics of North America. 2011;55(1):121-40. [ Links ]
15. Mandel L, Surattanont F. Regression of HIV parotid swellings after antiviral therapy: Case reports with computed tomographic scan evidence. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology and Endodontics. 2002;94(4):454-9. [ Links ]
16. Mulligan R, Navazesh M, Komaroff E, Greenspan D, Redford M, Alves M, et al. Salivary gland disease in human immunodeficiency virus-positive women from the WIHS study. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics. 2000;89(6):702-9. [ Links ]
17. Casiglia JW, Woo S-B. Oral manifestations of HIV infection. Clinics in Dermatology.18(5):541-51. [ Links ]
18. Islam NM, Bhattacharyya I, Cohen DM. Salivary gland pathology in HIV patients. Diagnostic Histopathology. 2012;18(9):366-72. [ Links ]
19. Monama GM, Tshifularo MI. Intralesional bleomycin injections in the treatment of benign lymphoepithelial cysts of the parotid gland in HIV-positive patients: Case reports. The Laryngoscope. 2010;120(2):243-6. [ Links ]
20. Favia G, Capodiferro S, Scivetti M, Lacaita MG, Filosa A, Muzio LL. Multiple parotid lymphoepithelial cysts in patients with HIV-infection: report of two cases. Oral Diseases. 2004;10(3):151-4. [ Links ]
21. Carlson ER. Diagnosis and Management of Salivary Gland Infections. Oral and Maxillofacial Surgery Clinics of North America. 2009;21(3):293-312. [ Links ]
22. Kim TB PS, Goldberg AN. Head and Neck Manifestations in the Immunocompromised Host. In: Flint PW, editor. Cummings Otolaryngology: Head & Neck Surgery. General Otolaryngology. 1. Fifth Edition ed. Philadelphia: Mosby; 2005. p. 209- 29. [ Links ]
23. Gurney TA, Murr AH. Otolaryngologic manifestations of human immunodeficiency virus infection. Otolaryngologic Clinics of North America. 2003;36(4):607-24. [ Links ]
24. Kabenge C, Ng S, Muyinda Z, Ameda F. Diagnostic ultrasound patterns of parotid glands in human immunodeficiency viruspositive patients in Mulago, Uganda. Dentomaxillofac Radiol. 2010;39(7):389-99. PubMed PMID: WOS:000281761200001. English. [ Links ]
25. Madani G, Beale T. Inflammatory conditions of the salivary glands. Seminars in Ultrasound, CT, and MRI. 2006;27(6):440-51. [ Links ]
26. Williams FM, Cohen PR, Jumshyd J, Reveille JD. Prevalence of the diffuse infiltrative lymphocytosis syndrome among human immunodeficiency virus type 1 positive outpatients. Arthritis & Rheumatism. 1998;41(5):863-8. [ Links ]
27. Itescu S, Brancato LJ, Buxbaum J, Gregersen PK, Rizk CC, Croxson TS, et al. A diffuse infiltrative CD8 lymphocytosis syndrome in human immunodeficiency virus (HIV) infection: a host immune response associated with HLA-DR5. Annals of Internal Medicine. 1990;112(1):3-10. [ Links ]
28. Rubinstein A, Morecki R, Silverman B, Charytan M, Krieger BZ, Andiman W, et al. Pulmonary disease in children with acquired immune deficiency syndrome and AIDS-related complex. The Journal of Pediatrics. 1986;108(4):498-503. [ Links ]
29. Yen TL, Murr AH, Rabin J, Mhatre AN, Lalwani AK. Role of Cytomegalovirus, Epstein Barr Virus, and Human Herpes Virus 8 in Benign Lymphoepithelial Cysts of the Parotid Gland. The Laryngoscope. 2004;114(8):1500-5. [ Links ]
30. Meyer E, Lubbe DE, Fagan JJ. Alcohol sclerotherapy of human immunodeficiency virus-related parotid lymphoepithelial cysts. The Journal of Laryngology & Otology. 2009;123(04):422-5. [ Links ]
31. Syebele K, Bütow K-W. Comparative study of the effect of antiretroviral therapy on benign lymphoepithelial cyst of parotid glands and ranulas in HIV-positive patients. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics. 2011;111(2):205-10. [ Links ]
32. Smith JA. HIV and AIDS in the adolescent and adult: An update for the Oral and Maxillofacial Surgeon. Oral and Maxillofacial Surgery Clinics of North America. 2008;20(4):535-65. [ Links ]
33. Patton LL, McKaig R, Strauss R, Rogers D, Eron Jr JJ. Changing prevalence of oral manifestations of human immuno-deficiency virus in the era of protease inhibitor therapy. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics. 2000;89(3):299-304. [ Links ]
34. Taiwo O, Hassan Z. The impact of Highly Active Antiretroviral Therapy (HAART) on the clinical features of HIV - related oral lesions in Nigeria. AIDS Research and Therapy. 2010;7(1):19. PubMed PMID: doi:10.1186/1742-6405-7-19. [ Links ]
35. Hegarty AM, Chaudhry SI, Hodgson TA. Oral healthcare for HIV-infected patients: an international perspective. Expert Opinion on Pharmacotherapy. 2008;9(3):387-404. [ Links ]
36. Basu D, Williams FM, Ahn CW, Reveille JD. Changing spectrum of the diffuse infiltrative lymphocytosis syndrome. Arthritis Care & Research. 2006;55(3):466-72. [ Links ]
37. Mandel L, Vakkas J. Parotid enlargement in patient with HIV. The New York State Dental Journal. 2005;71(1):44-6. [ Links ]
38. Patton LL, van der Horst C. Oral infections and other manifestations of HIV disease. Infectious Disease Clinics of North America. 1999;13(4):879-900. [ Links ]
39. Cunningham CM. Human immunodeficiency virus/acquired immune deficiency syndrome: the forgotten crisis and implications for the general surgery practice. The American Journal of Surgery. 2011;201(5):705-6. [ Links ]
40. Saltzman DJ, Williams RA, Gelfand DV, Wilson SE. The surgeon and AIDS: twenty years later. Archives of Surgery. 2005;140(10):961-7. [ Links ]
41. Martinson NA, Omar T, Gray GE, Vermaak JS, Badicel M, Degiannis E, et al. High rates of HIV in surgical patients in Soweto, South Africa: impact on resource utilisation and recommendations for HIV testing. Transactions of the Royal Society of Tropical Medicine and Hygiene. 2007;101(2):176-82. [ Links ]
 Correspondence:
Correspondence:
S Ebrahim
Departments of Surgery,
Nelson R. Mandela School of Medicine
University of KwaZulu-Natal
Private Bag 7
Congella
South Africa 4013
Cell: 082 485 8344, Fax: 086 593 0999
E-mail: ebrahims@ukzn.ac.za













