Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Dental Journal
versão On-line ISSN 0375-1562
versão impressa ISSN 0011-8516
S. Afr. dent. j. vol.69 no.7 Johannesburg 2014
RESEARCH
A comparison of preload values in gold and titanium dental implant retaining screws
R DoolabhI; HD DullabhII; LM SykesIII
IBDS, MSc (Dent). Registrar, Department of Prosthodontics, University of Pretoria
IIBChD, MSc, MDent. Professor and Head of Department, Department of Prosthodontics, University of Pretoria
IIIBSc, BDS, MDent. Principal Specialist and Associate Professor, Department of Prosthodontics, University of Pretoria
ABSTRACT
This in vitro investigation compared the effect of using either gold or titanium retaining screws on preload in the dental implant- abutment complex. Inadequate preload can result in screw loosening, whilst fracture may occur if preload is excessive. These are the most commonly reported complications in implant-retained prostheses, and result in unscheduled, costly and time-consuming visits for the patient and the clinician. This study investigated changes in preload generation after repeated torque applications to gold and titanium screws. The test set-up consisted of an implant body, a cylindrical transmucosal abutment, and the test samples of gold and of titanium retaining screws. The implant bodies were anchored using a load cell, and the transmucosal abutments were attached using either gold or titanium retaining screws. A torque gauge was used to apply torque of 20Ncm, 32Ncm, and 40Ncm to the retaining screws. The preloads generated in each screw type were compared at each torque setting, and after repeated tightening episodes. In addition, the effect of applying torque beyond the manufacturers' recommendations was also examined. Gold retaining screws were found to achieve consistently higher preload values than titanium retaining screws. Preload values were not significantly different from the first to the tenth torque cycle. Titanium screws showed more consistent preload values, albeit lower than those of the gold screws. However due to possible galling of the internal thread of the implant body by titanium screws, gold screws remain the retaining screw of choice. Based on the findings of this study, gold retaining screws generate better preload than titanium. Torque beyond the manufacturers' recommendations resulted in a more stable implant complex. However, further investigations, with torque applications repeated until screw breakage, are needed to advise on ideal maintenance protocols.
INTRODUCTION
Osseointegrated implants have revolutionized the options of clinicians in restorative dentistry. Physiological success is dependent on the integration of the implant within the surrounding osseous tissue, while prosthodontic success relies on a good mechanical fit between the components within the implant-abutment-prosthesis complex.1 In screw-retained restorations, the screw is responsible for clamping the transmucosal abutment to the implant fixture, and predictable longterm success relies on the integrity of that screw joint.
Literature review
The retaining screw connects the transmucosal abutment to the implant body and confers the advantages of retrievability, and of allowing for periodic implant and soft tissue assessment, the debridement of calculus, and prosthetic modifications or repairs.2 The screws are designed to loosen or fracture before damage to the implant fixture or overlying prosthesis occurs.3 This fail-safe characteristic is due to their reduced size, metallurgical composition, and the biomechanical parameters of the screw joint assembly.4,5
Application of torque to the retaining screw causes elongation and the subsequent elastic recovery results in the generation of a compressive clamping force.6 The tension thus created in the retaining screw during tightening is defined as the preload.7 Maintenance of an optimum preload in the screw joint is of critical importance to ensure the long term functioning of the implant- abutment- complex and to minimize fatigue in the screws.8 Inadequate preload results in increased wear and accelerates fatigue of the screw. Metal fatigue is the most common cause of structural failure and occurs after repeated loading even though such loading occurs at stress levels below the maximum tensile strength of a material.9
Preload is affected by many factors, including torque applied to the screw, type of screw alloy, screw head design, abutment alloy, abutment surface and the presence of lubricants.10 The greater the torque applied the greater the preload generated. Size and surface area of the contacting threads, pitch, screw radius and diameter of the head play major roles in the relationship between applied torque and preload.11 Surface area contact is also dependent on length of the screw, which determines the number of thread surfaces engaging. Frictional forces acting on these interfaces affect the relation between preload and applied torque. The amount of friction depends on the geometry and material properties of the interfaces, with additional energy being needed to overcome these forces.10
Screw loosening following functional loading has been cited as the most common mechanical complication for implant supported prostheses, and may be an early indicator of design inadequacies.1,12 The resulting micro-movement at the implant interface may lead to mechanical irritation of the surrounding soft tissues, gingival tenderness, bacterial colonization, inflammation, hyperplasia and later fistula formation with peri-implantitis.13 Fracture of the overlying prostheses and implant body fracture have also been reported.1 These complications result in costly and time-consuming unscheduled visits.8 Screw loosening occurs when the axial and bending moments acting on the screw (joint separating forces), generated by the cyclic forces of mastication, are greater than the clamping force.14 These displacing forces are amplified by excursive contacts, off-axis centric contacts, interproximal contacts, long cantilevers, lack of a passively engaging prostheses, and parafunctional habits.2,13,15 From an engineering perspective, screw loosening and/ or fracture may be attributed to inaccurate or inadequate machining tolerances, inappropriate component materials, metal fatigue, micro-movement during function, and the settling of screws. This settling effect or embedment relaxation occurs when the surface asperities produced during milling and tapping of the retaining screws are burnished with the initial application of torque.16,17 It has been reported that 2% to 10% of preload is lost within ten minutes of the initial torque application.9,18 To mitigate the problem of screw loosening, screw designs have been modified for improved performance, although the optimum design has not yet been fully established. Current designs generally consist of a flat head seat (for less frictional resistance and higher preload), long stem length (for optimal elongation and preload) and six threads to reduce friction because the first three threads carry most of the load,19 with the maximal stress being concentrated between the shank and first thread.20
The incidence of reported screw loosening is variable but is high, with a recorded 65% of screws in single tooth implants becoming loose within the first three years.2 Screw loosening within the first year is the most common problem for 42% of maxillary and 27% of mandibular prostheses.13, 20-23
The most commonly utilised retaining screws are constructed of either gold or titanium. Gold screws were designed to be the most "flexible" portion of the implant assembly due to their higher modulus of elasticity, which permits a degree of micro-movement, and distribution of forces.4 This design attribute also makes them the "weakest link" in the implant-abutment complex. In cases of occlusal overload the gold screw will fracture first, thus protecting the implant and underlying bone from excessive stresses.3 Gold screws can in fact attain a preload almost twice that of titanium alloy screws,19 but are weaker and will fracture due to metal fatigue sooner than titanium.4 The latter are stronger but their main disadvantage is the large frictional resistance between mating male and female threads, which has a tendency to cause galling.16,17 Galling is defined as the condition where excessive friction between two mating surfaces results in localized welding and roughening of the mating surfaces. It occurs when the titanium surfaces of the retaining screw and implant body slide in contact with each other. There is generation of increased friction that leads to transfer of titanium molecules from the mating surfaces, causing damage to both.8,16 Conversely, gold retaining screws have a smaller coefficient of friction, and can be tightened more effectively than titanium without risking galling between threads.
Screw tightening aims to generate an optimum preload that will maximise the fatigue life of the retaining screw, but at the same time offer protection against loosening.8 An optimal preload is important to maximize the frictional forces between mating threads and to ensure the stability of the implant complex. There is a difference between optimum torque, which is that torque which achieves an optimum preload, and the design torque specified by the manufacturer as being that needed to achieve optimum preload. Design torque is based on the nominal properties of the retaining screw and is calculated at 75% of ultimate torque-to-failure values.24 Manufacturer recommended values usually do not approach full design torque, as they have established a safety margin to optimise preload whilst decreasing the risk of screw fracture. Metallurgical properties of titanium screws allow for the generation of a more consistent, albeit lower, preload than with gold retaining screws. Recommended torque values of below 57.5% of the yield strength for gold alloy screws and 56% for titanium screws have been advocated.19 In a separate study, a preload of 75% of yield strength was not established using recommended tightening torque values.25 Despite these findings, torque cannot be applied arbitrarily without due consideration being given to the elastic limit of the screw and the biomechanics of the bone implant interface.16,17 If too much torque is applied to the implant complex, loss of integration at the implant-bone interface can occur.26 The retaining screw can also fail if torque is applied beyond its yield strength27 and threads can be stripped.2
The manner in which torque is delivered to the system is also important to ensure consistency. Variations have been found between hand screwdrivers, torque wrenches and electronic torque drivers, the latter being the most consistent when regularly calibrated.10 There are currently no suggestions for the torque that can safely be applied to the retaining screw beyond the manufacturers' recommendations. It is difficult to predict the fatigue life of retaining screws because of the differing material fatigue rates, and variable intra-oral loads. The estimated fatigue life of an implant screw has been reported to be about 20 years.9 Other authors agreed and stated that gold retaining screws can be removed and tightened up to 20 times with no effect on their tensile strength28, and suggested re-torquing within the first 3-12 months to compensate for embedment relaxation. Opinions differ as to how often screws should be retightened thereafter. However, to avoid fracture the critical number of torque cycles must not be exceeded.13,28 Screw thread deterioration after 4 to 10 years has been noted, hence the recommendation that retaining screws be replaced every 10 years.16 Other workers suggest replacement of gold screws during the lifetime of the restoration with no further detail given.4 There seems to be little consensus in the literature regarding maintenance protocols for abutment screws.
Abutment screws have either slotted, square, star or hexagonal driver engagement. A guiding effect can be achieved with the geometric designed engagements, resulting in more effective force transfer and greater stability, while it may be more difficult to apply manual force when tightening the slotted screws as clinicians are "anxious" to avoid slippage of the driver from the slot.13 The slotted, flat head retaining screw was investigated in this study because this design is commonly used in practice
AIM
The aim of this study was to evaluate the preload generated in gold and in titanium retaining screws and the effect of repeated torque on this preload.
MATERIALS AND METHOD
This was an in vitro laboratory study. An unused stack of components of the same batch (lot number 07A07/1) from one manufacturer (Southern Implants, Irene, South Africa) was used in this experiment to reduce the variations that occur between different lots and manufacturers. The test set-up consisted of:
- an implant body,
- a cylindrical transmucosal abutment,
- the test retaining screws.
Two self-tapping external hexagon implant bodies of 5mm diameter and 13mm length were used (Southern Implants, BA13 lot number 06051801/2). Each external hexagon was 2mm in height. The external hexagon has been shown to increase resistance to screw loosening,29 while the 2mm height is considered the most effective in dispersing lateral and bending forces through to the hexagon corners, thereby securing the preload in the retaining screw.27 Two titanium cylindrical transmucosal abutments (TCBASnh, lot number 0 6 0 5 1 8 01 /2 , SouthernImplants) designed for use with single implant restorations, were attached to the implant body with the retaining screws (Figure 1).
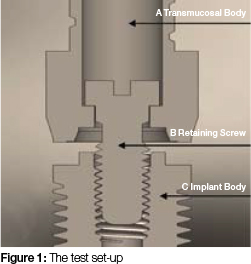
The test sample consisted of twenty slotted retaining screws. Ten were titanium (TSS2, alloy composition 90% Ti, 6% Al, 4% Vn) and ten were gold (GSS2, alloy composition 61% Au, 16.5% Ag, 13.5% Pt, 9% Cu). Each group of screws was tested using a new implant body and cylindrical transmucosal abutment.
A load cell (Loadtech, model number LT-400, South Africa), comprising of a central adjustable clamp for fixation of the implant body and a horizontal plate housing the cylindrical transmucosal abutment and retaining screw was used to measure preload in the screw (Figure 2). Preload was measured digitally in kilograms.

Torque was delivered to the system using an implant driver (I-WI-BL, Southern Implants), which was slotted into a torque gauge (Tohnichi, Japan, model BTG 150 CN, serial number 501935T) (Figure 3). The torque gauge and load cell were calibrated using known loads to give accurate and reproducible recordings prior to testing. All tests were performed in an airconditioned environment set at 25o C. Tests were performed by a single operator to ensure consistency in recording of data. Retaining screws were carefully handled throughout testing using plastic tweezers to ensure that no operatorinduced damage to the thread occurred. Screw torque was delivered in a steady manner by stabilizing and holding the head of the driver vertically with one hand, while the other hand applied the torque force to the torque gauge.

The procedure was as follows:
An initial torque of 20Ncm was applied to the retaining screw, that being the recommended tightening torque for TSS2. After a two minute waiting period to allow for embedment relaxation, 20 Ncm torque was re-applied to the screw and a reading was captured. After 30 seconds torque was increased to 32Ncm (as per manufacturers' recommendation for GSS2) and data was captured. After a further 30 seconds torque was applied up to 40Ncm and data captured. The purpose of the time intervals between applications of torque was to permit some settling, so that at the next torque application there would be better contact between mating surfaces allowing for a greater preload value. The three torque levels correspond to 62.5%, 100% and 125% of manufacturer's recommendations respectively. This process was repeated ten times per screw at each of the selected torque values, with the screw being removed and replaced at each cycle.
Statistical analysis
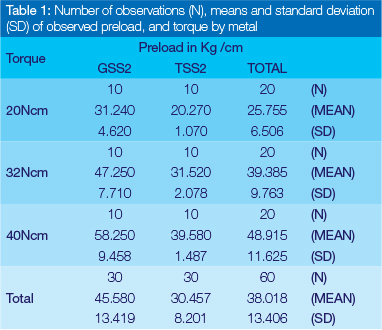
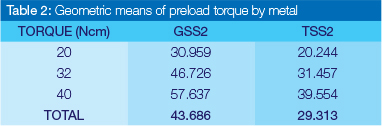
Preload values for each group of screws were obtained at each of the specified torque values (20Ncm, 32Ncm and 40 Ncm). For preload values during the first cycle, the mean and the standard deviation for each metal-torque combination as well the marginal values (i.e. the metals value divided by the torque measurements) were calculated (Table 1). The preload data was subjected to an analysis of variance (ANOVA) for repeated measures in the first cycle analysing preload on the (natural) logarithmic scale. ANOVA showed that the performance of the metals differed significantly (p < 0.0001). Geometric means were calculated as the antilog of the mean of the log values and hence the geometric mean of gold is significantly higher than that of titanium, 43.7Ncm as opposed to 29.3Ncm, as illustrated in Table 2.
To determine whether there was an inherent difference in the qualities of the different screw types, a final analysis comparing the two screw types with respect to the changes in preload from 20Ncm torque in the first cycle to 40Ncm torque in the tenth cycle was done using an analysis of covariance (ANCOVA) with the value at 20Ncm torque in the first cycle used as baseline covariate. The two metals did not differ significantly with respect to the mean change in preload, adjusted for baseline, (p=0.5159: 18.7 for GSS2 and 16.9 for TSS2).
RESULTS
For titanium, the mean value of the preloads measured at each sequence of ten torque cycles were 20.270Ncm, 31.520Ncm and 39.580Ncm at 20Ncm, 32Ncm and 40Ncm respectively, while for gold the values were 31.240Ncm, 47.250Ncm and 58.250Ncm (Figure 4). The mean preload value for all the torque cycles was 30,457Ncm for titanium and 45.580Ncm for gold. An ANOVA of the repeated measures in the first cycle (i.e. for each screw preload measured following torque measured at, respectively, 20Ncm, 32Ncm and 40Ncm) revealed that there was no significant difference between the metals (p < 0.0001).
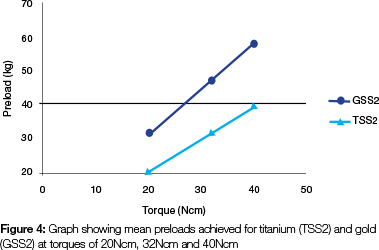
A further analysis was done to compare titanium to gold with respect to the change in preload from 20Ncm in the first cycle to 40Ncm in the tenth cycle, using an ANCOVA. This revealed that the metals were not significantly different (p> 0.5159), showing mean preloads of 16.9226Ncm for titanium and 18.6874Ncm for gold.
DISCUSSION
Screw loosening is a recognised problem in dental implant therapy. Retaining screws have been extensively studied and are constantly being improved upon. They are limited by size, material properties and maximum torque tolerance. The gold screw was originally designed to withstand only 10Ncm of torque (corresponding to that force which can be generated by hand tightening), and were intended to be the "weakest link" that would fracture first before damage to the prosthesis or implant body could occur.21 Screw loosening results from cyclic forces of mastication causing repeated deformation of the screw. This is compounded by a loss of preload due to embedment relaxation (the settling effect) where energy is expended in the burnishing of surface asperities of mating surfaces caused during manufacturing.17 Up to 10% of the initial preload may be lost within the first two minutes.9 This loosening is initiated when the mating threads slip, termed the critical bending moment and subsequently the loss of preload reaches a threshold point where any vibration will allow the screw to back out.10
Many strategies have been suggested in the attempt to minimise screw loosening, most of which are focused on precision implant placement and appropriate prosthesis design. Implants should ideally be parallel to the applied occlusal forces with the prosthesis designed to direct those forces through the long axis of the implant.2 Further screw loosening can be limited by minimising cantilever length, eliminating posterior working and balancing contacts, centralising centric contacts, sharing anterior guidance with the natural dentition, engaging anti-rotational features and ensuring passively fitting frameworks.3
The results of this study indicated that material composition of the retaining screw significantly influenced the preload with the gold screws generating consistently higher preload values. This is in accord with previous studies, but preload figures in this study were slightly below the 2:1 ratio of gold to titanium shown by Tan et al (2004).19 This may be due to manufacturing differences.15 The gold screws had a higher modulus of elasticity and are "softer" than titanium, and thus generated higher preload values. This was partially attributed to more intimate mating of female and male threads. However, this "softness" results in long-term deformation of the threads and subsequent loss of preload after the first torque cycle, although it did remain reasonably constant thereafter. In contrast the smaller preloads generated by titanium screws remained unchanged during successive tightening episodes. However gold screws are still preferred because of the potential galling of the titanium screws. As the titanium slides in contact with titanium, the coefficient of friction is initially fairly low, but with repeated tightening and loosening, the values gradually increase, causing damage to the internal thread of the implant body.
Published preload values in retaining screws vary considerably among studies, which may be due to differences in the manufacturing processes, lot numbers, and experimental procedures followed. Some studies calculated preload from opening torque values,30 compression in the implant complex,31 or from rotational angles.8 This may account for the slightly lower preloads recorded here. The optimum preload recommended for the retaining screw is that which produces a stress level between 60% and 75% of the yield strength of the material.32 Preload that is equal to the ultimate tensile strength of the material results in tightening-induced stress and finally fracture of the retaining screw. Stress at or slightly above yield causes the retaining screw to function in the plastic deformation zone with resulting sub-optimal function and loss of preload. However, a preload within the elastic range of the material is the most appropriate in terms of resisting joint separating forces generated during occlusal loading. Furthermore, optimum preload maximises the fatigue life of the screw as the load is transferred from the abutment to the implant surface with minimal effect on the screw.5
In this study, torque beyond the manufacturers recommendations, corresponding to 125% of the stipulated torque, resulted in consistently higher preload values. However, one is still unsure as to whether this is within the elastic limit of the screw. In addition, the biomechanics of the clinical situation must be carefully evaluated before exceeding the manufacturers guidelines as debonding between the implant and bone interface can occur with forces as little as 30Ncm.26
There is a relationship between preload, screw design, and material property. Friction influences preload generation, especially when new components are used, as in this investigation where the results suggest that wear from repeated closing/opening cycles may decrease the coefficient of friction between the screw head, threads, and other mating components. Consequently, resistance to opening gradually decreases as the resultant preload values fall. The coefficient of friction is affected by the manufacturing process, the metallurgical properties of the components, design and quality of the surface finish. As the study was done under dry conditions, the results may differ in the clinical situation where oral fluids could act as a lubricant to decrease the coefficient of friction and allow for greater tightening. It then follows that the preload values in this study would be lower than those expected clinically.30 This will also be affected by how many times the prosthesis is inserted and removed clinically.
This study showed that higher preload values could be achieved using gold retaining screws with a higher torque. This may avoid the screw loosening, adverse soft tissue reactions, and loss of implant function associated with insufficient or reduction of preload. Limitations of this study are that the experimental screws were all from one manufacturer and the results may not be transferable to designs or items produced by other manufacturers. The number of torque cycles in this study was limited to ten and may have been insufficient to cause screw joint deterioration. Additionally, the study was conducted under dry and static conditions. Furthermore, the same implant body was used for each of the test groups. Particulate matter from the screw threads could have coated the implant internal threads, especially from the gold retaining screws, further reducing preload values. Considering the host of challenges in the oral environment, it is clear that this study understates the loss of preload that would occur clinically.
CONCLUSIONS AND RECOMMENDATIONS
Gold screws generate higher preload values than titanium. Torque of 40Ncm to the retaining screw results in consistently higher preload values, thus, depending on the clinical situation, torque beyond the manufacturers' recommendation (by 25%) can be safely applied to ensure a more stable screw joint.
References
1. Gratton D, Aquilino SA, Stanford CM. Micromotion and dynamic properties of the dental implant-abutment interface. J Prosthet Dent. 2001; 85: 47-52. [ Links ]
2. McGlumpy E, Mendel DA, Holloway JA. Implant screw mechanics. Dent Clinics North America. 1998; 42: 71-89. [ Links ]
3. Rangert B, Jemt T, Jorneus L. Forces and moments on Branemark Implants. Int J Oral Maxillofac Implants. 1989; 4: 241-7. [ Links ]
4. Weinberg, L., The biomechanics of force distribution in implant-supported prostheses. Int J Oral Maxillofac Implants.1993;8: 19-31. [ Links ]
5. Yousef, H, Luke, A, Ricci, J, Weiner, S. Analysis of changes in implant screws subject to occlusal loading: A preliminary analysis. Implant Dent. 2005;14: 378-85. [ Links ]
6. Wang R, Kang B, Lang LA, Razzoog ME. The dynamic natures of implant loading. J Prosthet Dent. 2009; 101: 359-71. [ Links ]
7. (GPT-8)., G.o.p.t., Glossary of prosthodontic terms (GPT-8) J Prosthet Dent 2005; 94:10-92. [ Links ]
8. Martin W, Woody RD, Miller BH, Miller AW. Implant abutment screw rotations for four different screw materials and surfaces. J Prosthet Dent. 2001; 86: 24-32. [ Links ]
9. Tzenakis G, Nagy WW, Fournelle RA, Dhuru VB. The effect of repeated torque and salivary contamination on the preload of slotted gold implant prosthetic screws. J Prosthet Dent. 2002; 88:183-91. [ Links ]
10. Tan K, Nicholls JI. The effect of three torque delivery systems on gold screw preload at the gold cylinder abutment screw joint. Int J Oral Maxillofac Implants. 2002; 17: 175-83. [ Links ]
11. Tan K, Nicholls JI. Implant-abutment screw joint preload of seven hex-top abutment systems. Int J Oral Maxillofac Implants. 2001;16:367-77. [ Links ]
12. Duncan J, Nazarova E, Voiatzi T, Taylor TD. Prosthodontic complications in a prospective clinical trial of single stage implants at 36 months. Int J Oral Maxillofac Implants. 2003;18: 561-5. [ Links ]
13. Kallus T, Bessing C. Loose gold screws frequently occur in full-arch fixed prostheses supported by osseointegrated implants after 5 years. IntJ Oral Maxillofac Implants. 1994;9: 169-78. [ Links ]
14. Jaarda M, Razzoog, ME, Gratton DG. Geometric comparison of five interchangeable implant prosthetic retaining screws. J Prosthet Dent. 1995; 74:373-9. [ Links ]
15. Rambhia S, Nagy WW, Fournelle RA, Dhuru VB. Defects in hexed gold prosthetic screws: A metallographic and tensile analysis. J Prosthet Dent. 2002; 87: 30-39. [ Links ]
16. Jabbari Y, Fournelle R, Ziebert G, Toth J, Iacopino AM. Mechanical behavior and failure analysis of prosthetic retaining screws after long-term use in vivo. Part 1: Characterization of adhesive wear and structure of retaining screws. J Prosthodont. 2008; 17: 168-80. [ Links ]
17. Jabbari Y, Fournelle R, Ziebert G, Toth J, Iacopino AM. Mechanical behavior and failure analysis of prosthetic retaining screws after long-term use in vivo. Part 2:Metallurgical and microhardness analysis. J Prosthodont. 2008;17:181-91. [ Links ]
18. Winkler S, Ring K, Ring JD, Boberick KG. Implant screw mechanics and the settling effect: an overview. J Oral Implantology. 2003; 29: 242-5. [ Links ]
19. Tan B, Tan KB, Nicholls JI. Critical bending moments of implant-abutment screw joint interfaces: Effect of torque levels and implant diameter. Int J Oral Maxillofac Implants. 2004;19: 648-58. [ Links ]
20. Alkan I, Sertgoz A, Ekici B. Influence of occlusal forces on stress distribution in preloaded dental implant screws. J Prosthet Dent. 2004; 91:319-25. [ Links ]
21. Jemt T, Laney WR, Harris D, Henry PJ, Krogh PHJ, Polizzi G. Osseointegrated implants for single tooth replacement: A 1-year report from a multicenter prospective study. Int J Oral Maxillofac Implants. 1991; 6: 29-36. [ Links ]
22. Naert I, Quirynen M van Steenberghe D, Darius P. A six-year prosthodontic study of 509 consecutively inserted implants for the treatment of partial edentulism. J Prosthet Dent.1990; 67: 236-45. [ Links ]
23. Goodacre C, Bernal G, Rungcharassaeng K, Kan JYK. Clinical complications with implants and implant prostheses. J Prosthet Dent. 2003; 90:121-32. [ Links ]
24. Burguete R, Johns RB, King T, Patterson EA. Tightening characteristics for screwed joints in osseointegrated dental implants. J Prosthet Dent. 1994;71: 592-9. [ Links ]
25. Lang L, Kang B, Wang RF, Lang BR. Finite element analysis to determine implant preload. J Prosthet Dent. 2003; 90:539-46. [ Links ]
26. Brunski J. In vivo bone response to biomechanical loading at the bone/dental-implant interface. Adv Dent Res. 1999; 13: 99-119. [ Links ]
27. Khraisat A, Hashimoto A, Nomura S, Miyakawa O. Effect of lateral loading on abutment screw loosening of an external hexagon implant system. J Prosthet Dent. 2004; 91: 326-34. [ Links ]
28. Rafee M, Nagy WW, Fournelle RA, Dhuru VB, Tzenakis GK, Pechous CE. The effect of repeated torque on the ultimate tensile strength of slotted gold prosthetic screws. J Prosthet Dent. 2002; 88:176-82. [ Links ]
29. Binon B. The effect of implant / abutment misfit on screw joint stability. Int J Prosthodont.1996; 9:149-60. [ Links ]
30. Weiss E, Kozak D, Gross MD. Effect of repeated closure on opening torque values in seven abutment-implant systems. J Prosthet Dent. 2000; 84:194-9. [ Links ]
31. Cantwell A, Hobkirk JA. Preload loss in gold prosthesis-retaining screws as a function of time. Int J Oral Maxillofac Implants. 2004; 19:124-32. [ Links ]
32. Guda T, Ross TA, Lang LA, Millwater HR. Probabilistic analysis of preload in the abutment screw of a dental implant complex. J Prosthet Dent. 2008; 100:183-93. [ Links ]
 Correspondence:
Correspondence:
LM Sykes:
Principal Specialist and Associate Professor
Department of Prosthodontics
University of Pretoria
Fax: +27 012 323 0561
E-mail: Leanne.sykes@up.ac.za













