Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Dental Journal
On-line version ISSN 0375-1562
Print version ISSN 0011-8516
S. Afr. dent. j. vol.69 n.7 Johannesburg 2014
CASE BOOK
Oral medicine case book 62: CREST syndrome
BK BunnI; AW van ZylII; L RahmanIII; WFP van HeerdenIV
IBDS, MDent, FC Path (SA)Oral Path. Department of Oral Pathology and Oral Biology, School of Dentistry, Faculty of Health Sciences, University of Pretoria
IIBChD, MChD. Department of Periodontics and Oral Medicine, School of Dentistry, Faculty of Health Sciences, University of Pretoria
IIIBChD. Department of Periodontics and Oral Medicine, School of Dentistry, Faculty of Health Sciences, University of Pretoria
IVBChD, MChD, FC Path (SA)Oral Path, PhD, DSc. Department of Oral Pathology and Oral Biology, School of Dentistry, Faculty of Health Sciences, University of Pretoria
CASE REPORT
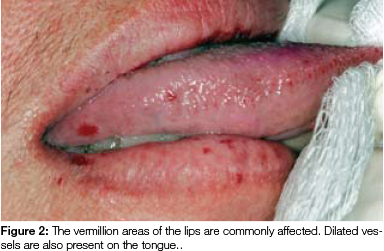
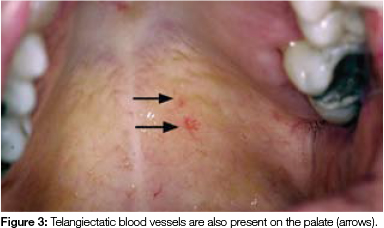
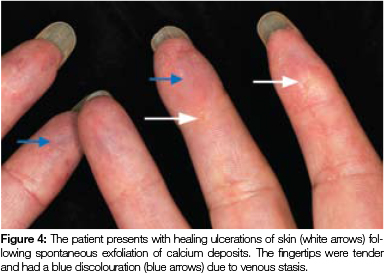
A 42-year-old female patient presented to the Department of Periodontics and Oral Medicine, with a main complaint of labial gingival recession on tooth 41. A comprehensive periodontal examination was performed with no findings of periodontitis. Gingival recession was found on teeth 41, 43, 45, 31, 34, and 13. Clinical examination of the intra-oral mucosa and peri-oral facial skin showed multifocal asymptomatic telangiectases (Figures 1 to 3). The patient disclosed a chronic history of Raynaud's phenomenon which was initially diagnosed in her early teens. In addition, there was evidence of sclerodactyly and focal areas of calcinosis cutis (calcinosis of the skin) (Figure 4). The patient complained of mild dysphagia and gastric reflux.

The severity and pain associated with her Raynaud's phenomenon, particularly on exposure to cold, had prompted the patient to consult a physician many years previously. At that time, laboratory testing had shown increased antinuclear antibody (ANA) titres. Some years later she consulted a rheumatologist, who diagnosed CREST syndrome on the basis of her clinical features and the presence of anti-centromeric antibodies on laboratory testing.
The patient was on antidepressant medication and occasionally took non-steroidal anti-inflammatory drugs for digital and joint pain. The Miller's Class II gingival recession of tooth 41 was surgically managed by means of a subepithelial connective tissue graft, using a microsurgical technique. Healing was uneventful.
DISCUSSION
The slowly progressive cutaneous form of systemic sclerosis (scleroderma) is termed CREST syndrome. The acronym CREST is derived from the clinical symptoms of Calcinosis of the skin, Raynaud's phenomenon, Esophageal dysmotility, Sclerodactyly and Telangiectasia.1 The oral manifestations of CREST syndrome are poorly documented. This case presentation aims to discuss a fairly rare clinical entity and the implications for dental management.
Scleroderma is contemporarily referred to as systemic sclerosis but remains a poorly defined, ill-understood form of autoimmune disease. It is characterised by sclerosis of the dermal connective tissue and occasionally involves the visceral organs. Vasculopathic involvement and increased circulating autoantibodies are typical features.1 A localised form of systemic sclerosis occurs in the cutaneous lesions of morphoea and linear scleroderma. Systemic sclerosis may occur as a diffuse condition or as the specific form denoted by the acronym CREST.1 Patients with CREST syndrome present with sclerodermatous changes of the oral mucosa and peri-oral soft tissue. They frequently complain of limited mouth opening and induration of the tongue with resultant speech and swallowing difficulty.1,2 Previous studies of periodontal disease in patients with systemic sclerosis have shown mucogingival involvement characterised by loss of attached gingiva and multifocal areas of gingival recession.1,3 The increased incidence of dental caries and periodontitis encountered in these patients necessitates a greater need for prophylactic plaque control measures and preventative dental management. Patients may also suffer from xerostomia as a result of Sjögren's syndrome (SS).
CLINICAL CHARACTERISTICS
Calcinosis: Soft tissue deposition of calcium in CREST in CREST syndrome are a late manifestation of the disease process and are unrelated to disorders of calcium metabolism.1,4 Calcium deposits are noted within the extremities and occur superficially within the dermal connective tissue. They rarely interfere with patient function and seldom require additional therapy.
Raynaud's phenomenon: Raynaud's phenomenon is usually the earliest manifestation of CREST syndrome and represents a vasomotor disorder affecting the extremities. Patients suffer from vascular spasms of the acral arteries which are induced by exposure to cold. The vascular spasm results in decreased peripheral perfusion which may last several minutes followed by painful re-perfusion. Vasoactive medication in the form of calcium channel blockers can be used to alleviate these symptoms in only the most severe cases.5 Generalised gingival overgrowth may result from administration of this medication and further complicate plaque control and periodontal involvement.1
ACRONYMS
ANA: Antinuclear antibodies
CREST: Calcinosis of the skin, Raynaud's phenomenon, Esophageal dysmotility, Sclerodactyly and Telangiectasia
GERD: Gastro-esophageal reflux disease
SS: Sjögren's syndrome
Esophageal dysmotility: Esophageal involvement in CREST syndrome is due to smooth muscle atrophy and fibrosis which results in uncoordinated contraction, dysphagia and gastroesophageal reflux disease (GERD).2,6 Severe chemical erosion of tooth enamel may result from chronic GERD.
Sclerodactyly: The tightening of the skin with tapering of the fingers and toes is termed sclerodactyly. The most severely affected digits may show clinical features of contracture. Initial clinical changes include oedema followed by atrophy and thinning of the skin. The fingers become progressively rigid which may result in a loss of dexterity which may interfere with the patient's ability to manually perform plaque control measures.1
Telangiectases: Telangiectatic lesions in CREST syndrome are usually noted to involve the oral and gastro-intestinal mucosa as well as the skin of the trunk and extremities. Unlike the hereditary telangiectatic lesions seen in Rendu-Osler Weber disease, there is no association with haemorrhagic episodes in CREST syndrome. Lesions appear to increase in number as patients' age but are largely asymptomatic.7
The diagnosis of CREST syndrome is often delayed as the disorder is slowly progressive and not all features are present from the outset. Laboratory detection of ANA's, in particular anti-centromeric antibody, is supportive of the clinical diagnosis. The oral health care worker should also be aware that patients with CREST syndrome have a higher incidence of associated auto-immune disease, notably of SS.1 The xerostomia occurring in SS further complicates the oral manifestations of CREST.
The soft tissue changes seen in CREST syndrome become progressively more severe over prolonged periods of time. Plaque control becomes more difficult for patients to manage. Early clinical recognition and diagnosis together with the institution of regular dental examinations and a rigorous plaque control programme may serve to prevent or at the very least delay the onset of periodontal disease and dental caries in this group of patients.
CONCLUSION
CREST syndrome is a rare form of auto-immune disease. An interesting example of a patient with this disorder is presented here to highlight the oral manifestations as well the importance of optimal plaque control in these patients. Appropriate referral of patients to specialist physicians and rheumatologists may be necessary for systemic immunosuppressive therapy.
Declaration: No conflict of interest declared.
References
1. Stanford TW, Jr., Peterson J, Machen RL. CREST syndrome and periodontal surgery: a case report. J Periodontol 1999; 70: 536-41. [ Links ]
2. Nisa L, Giger R. Dysphagia, oral telangiectasia, and Raynaud syndrome. Otolaryngol Head Neck Surg 2012; 146: 676-7. [ Links ]
3. Eversole LR, Jacobsen PL, Stone CE. Oral and gingival changes in systemic sclerosis (scleroderma). J Periodontol 1984; 55: 175-8. [ Links ]
4. Selig HF, Pillukat T, Muhldorfer-Fodor M, Schmitt S, van Schoonhoven J. Surgical treatment of extensive subcutaneous calcification of the forearm in CREST syndrome. J Plast Reconstr Aesthet Surg 2013; 66: 1817-8. [ Links ]
5. Ennis H, Anderson ME, Wilkinson J, Herrick AL. Calcium channel blockers for primary Raynaud's phenomenon. Cochrane Database Syst Rev 2014; 1: CD002069. [ Links ]
6. Carr RD, Heisel EB, Stevenson TD. CREST syndrome. A benign variant of scleroderma. Arch Dermatol 1965; 92: 519-25. [ Links ]
7. Halachmi S, Gabari O, Cohen S, Koren R, Amitai DB, Lapidoth M. Telangiectasis in CREST syndrome and systemic sclerosis: correlation of clinical and pathological features with response to [ Links ]
 Correspondence:
Correspondence:
WFP van Heerden:
Department of Oral Pathology and Oral Biology
University of Pretoria
South Africa
Tel: +27 012 319 2320
Fax: +27 012 321 2225
E-mail: willie.vanheerden@up.ac.za













