Services on Demand
Journal
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SA Orthopaedic Journal
On-line version ISSN 2309-8309Print version ISSN 1681-150X
SA orthop. j. vol.13 n.3 Centurion Sep. 2014
FOOT AND ANKLE
Venous thromboembolic disease in hallux surgery
NP SaragasI; PNF FerraoII; E SaragasIII; BF JacobsonIV
IMBBCh(Wits), FCS(SA)Ortho, MMed(Ortho Surg)(Wits); Netcare Linksfield Orthopaedic Sports & Rehabilitation Centre (Clinic), Johannesburg; Orthopaedic Department, University of the Witwatersrand, Johannesburg, South Africa
IIMBChB(Pret), FCS(SA)Ortho; Netcare Linksfield Orthopaedic Sports & Rehabilitation Centre (Clinic), Johannesburg; Orthopaedic Department, University of the Witwatersrand, Johannesburg, South Africa
IIIMBBCh(Wits), FFPath(Haem)(SA); Department of Molecular Medicine and Haematology School of Pathology, Faculty of Health Sciences of the University of the Witwatersrand, Johannesburg, and National Health Laboratory Services
IVMBChB(Pret), MMed(Haem), FRCS(Glasg), FCPath(SA), PhD(Med); Department of Molecular Medicine and Haematology School of Pathology, Faculty of Health Sciences of the University of the Witwatersrand, Johannesburg, and National Health Laboratory Services
ABSTRACT
INTRODUCTION: Hallux surgery is the most commonly performed elective surgery in the foot and ankle. As with all surgery, there are many potential complications quoted in the literature. Venous thromboembolism (deep vein thrombosis and pulmonary embolism) prophylaxis, however, is not adequately addressed and remains controversial.
MATERIALS AND METHOD: This prospective study includes 100 patients who underwent hallux surgery. Risk factors implicated to increase the risk of developing venous thromboembolic disease as well as anaesthetic time, thigh tourniquet time and regional anaesthetic blocks were documented. Compressive ultrasonography was performed in all the patients post-operatively.
RESULTS: There was one incident of calf deep vein thrombosis (DVT). No patient developed a pulmonary embolus. The one patient who developed a DVT was not at any higher risk than the average patient in the study.
CONCLUSION: As a result of the low incidence of venous thromboembolic disease in this study, the authors do not recommend the routine use of chemical venous thrombo-prophylaxis in patients undergoing hallux surgery. The decision to give post-operative anticoagulation remains the surgeon's responsibility. The duration of prophylaxis will depend on when the patient is fully mobile.
LEVEL: 2
Keywords: hallux surgery, venous thromboembolism.
Introduction
Hallux surgery, with its varying degrees of complexity, is the most common elective surgery performed on the foot and ankle.
The complications and potential risks of hallux surgery in general, are well described in standard text books. However venous thromboembolism (deep vein thrombosis and pulmonary embolism) is inadequately addressed. There is a paucity of discussion in current literature with few prospective studies which are limited to hallux valgus surgery.1,2
In related articles, the incidence of venous thromboembolism (VTE) is mentioned as a complication in hallux valgus surgery.3-6
Radl et al. found an incidence of 4% deep vein thrombosis (DVT) and concluded that the risk of post-operative DVT should be assessed according to patient-related risk factors. They highlighted that patients over the age of 60 years may benefit from medical prophylaxis.1 This is in keeping with several other studies.7-14
There is also data to show that the incidence is even lower.2
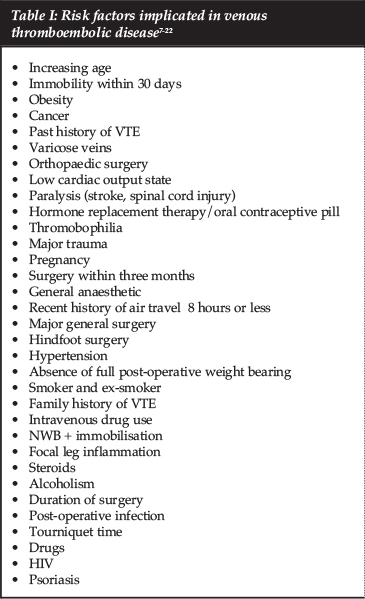
Besides age, many other risk factors have been implicated in venous thromboembolic disease (Table 1).7-22
The purpose of this prospective study was to determine the incidence of VTE and hence the need for chemical prophylaxis in hallux surgery.
Materials and method
The inclusion criteria were all consecutive patients requiring hallux surgery (hallux valgus correction, first metatarsophalangeal joint [MPJ] replacement and first metatarsophalangeal joint arthrodesis), from 2011 to 2013. All patients were 18 years and older.
Exclusion criteria were patients already on anticoagulants, previous venous thromboembolic disease and patients requesting anticoagulation.
Human Research Ethics Committee (Medical) approved the study (Clearance Certificate M110625).
All patients completed a 'Thrombosis Risk Factor Assessment' form, which has been endorsed by the Southern African Society of Thrombosis and Haemostasis (SASTH) (Figure 1).
The purpose of this prospective study was to determine the incidence of VTE and hence the need for chemical prophylaxis in hallux surgery
History of smoking, anaesthetic time, thigh tourniquet time and regional anaesthetic block were recorded, in addition to the above risk factors.
One hundred (92 females and eight males) consecutive patients (146 feet) were eligible for inclusion. The mean age was 54.1 years (range 18 to 79 years). Clinical examination for DVT was performed post-operatively while in hospital and at every follow-up visit (at 1, 2, 4, 6 weeks).
All patients were routinely subjected to compression ultra-sonography23 between two and six weeks post-operatively.
Results
There were 130 hallux valgus corrections (viz. Lapidus [34]; proximal open wedge [13], scarf [18], chevron [67] and Akin [76] osteotomies), 10 hallux MPJ arthrodesis and 6 MPJ replacements).
Associated forefoot surgery (viz. hammer toe and mallet toe corrections; interdigital neuroma excision; Weil osteotomies; bunionette resections and interphalangeal fusion) was performed in 38 patients.
Regional blocks were used in 146 limbs (72 popliteal and 74 ankle blocks) in conjunction with the general anaesthetic.
Average anaesthetic time was 108 minutes (range 45 to 210 minutes) and average thigh tourniquet time was 59 minutes (range 20 to 135 minutes).
The total risk factor score was 5.1 (range 2 to 10). The total risk factor score is the score that determines the risk of developing a DVT. This is calculated from the thrombosis risk factor assessment form. The higher the score, the higher the risk.
There was one (1%) incident of a symptomatic DVT (calf) one week post-operatively. Our one patient who developed a DVT was a female who had a unilateral Lapidus procedure and an associated interdigital neuroma excision. The anaesthetic time was 105 minutes and tourniquet time 94 minutes. Her total risk factor score was 4. Her risk factors were age (54 years), BMI > 25 kg/m2 and length of surgery (greater than 45 minutes).
No patient developed pulmonary embolus.
Post-operatively all patients were mobilised on day one in a post-operative wedge heel shoe allowing them to bear weight on the heel as tolerated. No cast was used. This protocol included the patients who had bilateral surgery.
Discussion
Seventy-seven per cent of hip and knee surgeons routinely use thromboprophylaxis.24
This is understandable due to the high prevalence of DVT in total hip replacements (42-57%) and total knee replacements (41-85%).
In foot and ankle surgery, however, there is no consensus on the use of chemical thromboprophylaxis and there are no clear guidelines. This is particularly true for hallux surgery. This study has found a very low incidence of VTE.
In general, the recommendation for thromboprophylaxis is a total risk factor score of 5 or more, 5 being at the highest risk for developing DVT (incidence of 40-80%).7,25
Despite an average total risk factor score of 5.1, the incidence of DVT in our study group was very low (1%).
The authors feel that routine chemical thromboprophylaxis in hallux surgery per se is not warranted.
Individual patient specific risk factors, however, need to be assessed pre-operatively and measured against a validated scoring system. The decision to give postoperative anticoagulation remains the surgeon's responsibility, as large scale, prospective clinical trials are unlikely to be carried out due to financial constraints.
The duration of cover will depend on when the patient is fully mobile.
Conclusion
This current study does not recommend the routine use of chemical thromboprophylaxis in hallux surgery.
The emphasis therefore, is placed on individual, patient-specific risk factors. Furthermore, the total risk factor score guidelines may need to be revised in hallux surgery by increasing the sensitivity of the total score.
There is a need for larger prospective studies to identify the patient undergoing foot and/or ankle surgery who is a potential risk.
Acknowledgements
The authors wish to express their gratitude to Dr Diana Alagem from Diagnostic Radiological Services Inc. for performing the compression ultrasonography pro Deo, and to Mrs Wendy Leppan for the typing of the manuscript.
The authors declare no potential conflicts of interest with respect to the research, authorship and/or publication of this article. The authors received no financial support for the research, authorship and/or publication of this article.
References
1. Radl R, Kastner N, Aigner C, Portugaller H, Schreyer H, et al. Venous thrombosis after hallux valgus surgery. J Bone Joint Surg Am 2003;85:1204-208. [ Links ]
2. Simon MA, Mass DP, Zarins CK, Bidani N, Gudas CJ, et al. The effect of a thigh tourniquet on the incidence of deep vein thrombosis after opertions on the fore part of the foot. J Bone Joint Surg Am 1982 Feb;64(2):188-91. [ Links ]
3. Viladot R, Alvarado OJ, Arancibia M, Martinez JA, Ramirez JA, et al. Hallux valgus: A modified Kramer osteotomy. Foot and Ankle Surgery 2007;13(3):126-31. [ Links ]
4. Atlintas F, Ozler T, Güven M, Ozkut AT, Ulucay C. Deep venous thrombosis and pulmonary embolism as rare complications after hallux valgus surgery: case report and literature review. J Am Podiatr Med Assoc 2013 Mar-Apr;103(2):145-48. [ Links ]
5. Fridman R, Cain JD, Weil L Jr, Weil LS Sr Ray TB. Unilateral versus bilateral first ray surgery. A prospective study of 186 consecutive cases patient satisfaction, cost to society, and complications. Foot and Ankle Specialist 2009;2(3):123-29. [ Links ]
6. Lucijanić I, Cicvara-Pećina T, Bićanić G, Pećina M. [Simultaneous surgical correction of hallux valgus and lesser toes deformity] (Article in Croatian). Medica Jadertina 2011;41(3-4):105-11. [ Links ]
7. Jacobson BF, Louw S, Mer M, Haas S, Buller HR, Abdul-Carrim ATO. Venous thromboembolism - prophylactic and therapeutic practice guideline. SAMJ 2009;99(6):467-73. [ Links ]
8. Solis G, Saxby T. Incidence of DVT following surgery of the foot and ankle. Foot Ankle Int 2002;23(5):411-14. [ Links ]
9. Soohoo NF, Eagan M, Krenek L, Zingmond DS. Incidence and factors predicting pulmonary embolism and deep venous thrombosis following surgical treatment of ankle fractures. Foot and Ankle Surgery 2011;17:259-62. [ Links ]
10. Hirsh J. Prevention of venous thromboembolism. In: Hirsh J, editor. Guidelines for antithrombotic therapy. Ontario: BC Decker Inc. 2008; p.51. [ Links ]
11. Edmonds MJ, Crichton TJ, Runciman WB, Pradham M. Evidence-based risk factors for post-operative deep vein thrombosis. ANZ J Surg. 2004;74(12):1082-97. [ Links ]
12. Sikorski JM, Hampson WG, Staddon GE. The natural history and aetiology of deep vein thrombosis after total hip replacement. J Bone Joint Surg Br 1981;63-B:171-77. [ Links ]
13. Syed FF, Beeching NJ. Lower-limb deep-vein thrombosis in a general hospital: Risk factors, outcomes and the contribution of intravenous drug use. Q J Med. 2005; 92:139-45. [ Links ]
14. White RH. The epidemiology of venous thromboembolism. Circulation 2003;107:1-4-8. [ Links ]
15. Hanslow SS, Grujic L, Slater HK, Chen D. Thromboembolic disease after foot and ankle surgery. Foot Ankle Int. 2006;27(9):693-95. [ Links ]
16. Jørgensen PS, Warming T, Hansen K, Paltved C, Berg HV, Jensen R, et al. Low molecular weight heparin (Innohep) as thromboprophylaxis in outpatients with a plaster cast. A venographic controlled study. Thromb Res 2002;105:477-80. [ Links ]
17. Kock H, Schmit-Neuerburg KP. Thromboprophylaxis with low-molecular-weight heparin in outpatients with plaster cast immobilization of the leg. Lancet 1995;346:459-66. [ Links ]
18. Lapidus LJ, Rosfors S, Ponzer S, Levander C, Elvin A, Larfars G, et al. Prolonged thromboprophylaxis with dalteparin after surgical treatment of Achilles tendon rupture: a randomized, placebo-controlled study. Orthop Trauma 2007;21(1):52-57. [ Links ]
19. Lassen MR, Borris LC, Nakov RL. Use of the low-molecular-weight heparin reviparin to prevent deep-vein thrombosis after leg injury requiring immobilization. N Engl J Med 2002;347(10):726-30. [ Links ]
20. Mizel MS, Temple HT, Michelson JD, Alvarex RG, Clanton TO, Frey CC, et al. Thromboembolism after foot and ankle surgery. Clin Orthop 1998;348:180-85. [ Links ]
21. Goldhaber SZ, Tapson VF, DVT Free Steering Committee. A prospective registry of 5 451 patients with ultrasound -confirmed deep-vein thrombosis. Am J Cardiol 2004;15;93(2):259-62. [ Links ]
22. Ahlehoff O, Gislason GH; Lindhardsen J, Charlot MG, Jorgensen CH. Psoriasis carries an increased risk of venous thromboembolism: A Danish nationwide cohort study. PLoSone 2011;6(3):1-5. [ Links ]
23. Lapidus L, De Bri E, Ponzer S, Elvin A, Noren A, et al. High sensitivity with color duplex sonography in thrombosis screening after ankle fracture surgery. J Thromb Haemostat 2006;4:807-12. [ Links ]
24. Gadgil A, Thomas RH. Current trends in thromboprophylaxis in surgery of the foot and ankle. Foot Ankle Int 2007;28(10):1069-73. [ Links ]
25. Wessels PF, Riback WJ. DVT prophylaxis in relation to patient risk profiling - the TUNE-IN study. SAMJ 2012;102(2):85-89. [ Links ]
 Correspondence:
Correspondence:
Dr NP Saragas
PO Box 1153
2037 Highlands North
Johannesburg, South Africa
Tel: +27 11 485-1974/5
Fax: +27 11 640-5313
Email: saragas@global.co.za
This article is also available online on the SAOA website (www.saoa.org.za) and the SciELO website (www.scielo.org.za). Follow the directions on the Contents page of this journal to access it.













