Services on Demand
Journal
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.99 n.9 Pretoria Sep. 2009
ORGINAL ARTICLES
Estimation of adult antiretroviral treatment coverage in South Africa
Muhammad Aarif AdamI; Leigh F JohnsonII,*
IBBusSc, S Afr Med J 2009; 99: 661-667.Sanlam Life Insurance Limited, Bellville, W Cape
IIPhD, AIA, Centre for Actuarial Research, University of Cape Town
ABSTRACT
OBJETIVES: To estimate the annual numbers of individuals receiving antiretroviral treatment in South Africa up to mid-2008, and the coverage of antiretroviral treatment in adults according to various definitions of need.
METHODS: Antiretroviral coverage is defined as the number of patients receiving antiretroviral treatment at a point in time, divided by the number needing treatment. Numbers of patients receiving antiretroviral treatment are estimated from public sector data, and data provided by disease management programmes and NGO programmes. The unmet need for treatment in adults is estimated using a Markov model of HIV progression in adults, combined with estimates of annual new HIV infections from a national AIDS and demographic model.
RESULTS: By the middle of 2008, 568 000 adults and children were receiving antiretroviral treatment in South Africa, with the public health sector accounting for 79% of this total. Using the current Department of Health criteria for defining antiretroviral eligibility (CD4+ count <200/µl or World Health Organization (WHO) stage 4), antiretroviral coverage in adults was 40.2% in 2008 — up from 4.9% in 2004. Coverage increases to 54.2% if eligibility is based on WHO stage 4 only, but falls to 22.2% if the Southern African HIV Clinicians Society guidelines are used to define eligibility. Coverage in 2008 varied between provinces, from 25.8% in the Free State to 71.7%
CONCLUSIONS: Significant progress has been made in expanding access to antiretroviral treatment in South Africa since 2004, but a substantial unmet need for treatment in adults remains.
Death notification statistics confirm that AIDS is dramatically affecting mortality in South Africa.1 Demographic and epidemiological models suggest that antiretroviral treatment is the only intervention that can achieve a substantial reduction in AIDS mortality in South Africa in the short term.2,3 South Africa therefore urgently needs to expand and strengthen services providing antiretroviral treatment. Before 2004, access to antiretroviral drugs was limited mainly to medical scheme beneficiaries. However, following the announcement of a comprehensive care, management and treatment programme by the Department of Health (DoH) in late 2003,4 antiretroviral treatment has become increasingly accessible, and significant progress has been made in enrolling patients onto the public antiretroviral treatment programme.
Despite this progress, there remains a significant unmet need for antiretroviral treatment in South Africa; monitoring of antiretroviral coverage is therefore important to identify where the shortfall is greatest and to quantify coverage according to different definitions of 'need'. However, monitoring of antiretroviral coverage in South Africa is challenging for several reasons. Although the DoH regularly co-ordinates data collection for the public health sector, there is no centrally co-ordinated data collection system for the private sector and non-governmental organisations (NGOs). In addition, the numbers routinely reported by the DoH are the numbers of patients cumulatively enrolled on antiretroviral treatment, and there are no estimates of public-sector patients currently receiving antiretroviral treatment, except in the Western Cape. Coverage is also difficult to estimate because demographic projection models usually estimate only the numbers of individuals in different WHO clinical stages,2,5 whereas definitions of eligibility are usually based on a combination of clinical and CD4+ criteria.4,6,7 This makes it difficult to estimate the denominator in the antiretroviral coverage calculation.
Much is unknown regarding antiretroviral coverage in South Africa. The aim of this paper is to quantify the coverage in South Africa up to the middle of 2008, according to various definitions of antiretroviral treatment eligibility, and to quantify the relative levels of coverage in the nine provinces and the changing contribution of different providers to the antiretroviral rollout in South Africa.
Method
Following the convention of UNAIDS and the World Health Organization (WHO), antiretroviral coverage is calculated as the number of individuals receiving antiretroviral treatment, divided by the sum of the number of untreated individuals needing treatment and the number of treated individuals.8,9 Estimates of the numbers receiving treatment are obtained from public sector programme reports and data collected from the private sector, while estimates of the unmet need for treatment are derived from a model of HIV progression in HIV-infected individuals. Although numbers receiving treatment are calculated for both adults and children, antiretroviral coverage is calculated for adults only, since definitions of antiretroviral eligibility and rates of HIV progression differ between children and adults.
Estimation of numbers receiving antiretroviral treatment
Estimates of the numbers of patients starting antiretroviral treatment each year in public health facilities are obtained from unpublished reports of the cumulative numbers of patients who have started antiretroviral treatment at different times (Department of Health internal report dated 7 May 2009: National Strategic Plan for HIV and AIDS/CCMT monthly statistics, March 2009).10 To allow for mortality and loss to follow-up after starting treatment, rates of retention are applied to these annual numbers of individuals starting therapy. Based on estimates of retention in the Western Cape,11 it is assumed that the probability of remaining on treatment for the first 6 months after starting therapy is 0.895, and the annual probability of remaining on treatment thereafter is 0.935. The number of individuals receiving treatment at time t (in years) is thus calculated as:
where S(t—1) is the number of individuals starting treatment between time t — 1 and time t. It is assumed that individuals starting treatment between time t — 1 and time t do so, on average, at time t — ½.
Estimates of the numbers of patients receiving antiretroviral treatment through disease management programmes (DMPs), workplace treatment programmes (WPTPs) and NGO programmes operating outside of public health facilities are based on three data sources:
1. early published data from Aid for AIDS,12 which was treating approximately 80% of all antiretroviral patients in 2002 13
2. early data on NGO programmes operating before 2004 14
3. more recent data collected from individual programmes from 2005 to 2008. 15
Since programmes do not provide estimates at regular intervals, and since information is missing for some programmes during certain periods, estimates of numbers of patients receiving treatment at the middle of each year are obtained by using linear interpolation and extrapolation of estimates at other time points. The number of individuals starting treatment between time t — 1 and time t, S(t—1), is estimated by entering the private sector estimates of N(t—1) and N(t) into equation (1) and assuming that the rates of retention in the private sector16,17 are the same as those in the Western Cape.
For some years, data on the provincial distribution of treatment numbers are not available. In these years, we assumed that the proportion of individuals treated in a particular province, and for a given sector (private/public/NGO), was the same as that estimated in the most recent year. For the public and NGO sectors, the most recent provincial distributions are for 2008. For the private sector, a provincial distribution could be obtained only for 2003, based on a weighting of the 2003 population5 by the proportion of the population with medical cover18 and the proportion of medically insured individuals on antiretroviral treatment. 12
Estimation of unmet need for treatment
The unmet need for treatment was estimated by using a Markov model of HIV progression that divides HIV-infected adults into compartments based on their current CD4+ count, clinical status and current receipt of antiretroviral treatment (Fig. 1). The initial CD4 distribution of HIV-infected adults, at the time they acquire HIV, as well as the probabilities of transition between the HIV stages in Fig. 1, are set at the rates estimated by Hendriks et al.19 from men in Amsterdam from 1990 to 1996. These rates were selected from several other possible sources,19-22 because they produced an estimated median HIV survival time consistent with medians estimated for South Africa in other studies23,24 and because they produced a distribution of CD4+ counts in HIV-infected adults roughly consistent with the distributions observed in South African surveys. 25-27

Assumptions about the annual number of new adult HIV infections were obtained from the ASSA2003 AIDS and Demographic model.5 The model projects the change in the number of infected individuals in the different CD4 stages at monthly intervals, adding new infections and removing individuals who die or start antiretroviral treatment. Non-HIV mortality is set at a rate of 0.005 per annum, equal to the average non-HIV mortality rate in HIV-positive South African adults estimated by the ASSA2003 model. The numbers of adults starting antiretroviral treatment in each period are set at 90% of the S(t) estimates obtained previously, since approximately 10% of those receiving antiretroviral treatment are children. Based on data from South African treatment programmes,17,28,29 we assumed that 35% of adults starting treatment had already progressed to AIDS and the balance started therapy when their CD4+ count was <200/µl, prior to the development of clinical AIDS.
Estimates of unmet need are calculated according to three definitions:
1. conservative criteria that include only adults with untreated AIDS
2. current criteria used by the DOH,4 which include all adults with untreated AIDS or a CD4+ count <200/µl
3. criteria recommended by the Southern African HIV Clinicians Society,7 which include all adults with untreated AIDS or a CD4+ count <350/µl.
Sensitivity analysis
To assess the sensitivity of the unmet need estimates to key variables, the following plausible ranges of parameter values are considered. The proportion of adults starting treatment who have already progressed to AIDS is varied between 20% and 50%,17,28,29 and the rate at which individuals discontinue treatment owing to death or loss to follow-up is varied between 0.7 times and twice the rates estimated from the Western Cape data, based on variability in rates of retention observed within South Africa.28,30,31 The annual numbers of new HIV infections in adults are varied between the upper and lower limits of the 95% prediction intervals calculated in a previous uncertainty analysis.24 In addition, alternative estimates of rates of transition between CD4 stages are considered. 19-22
Results
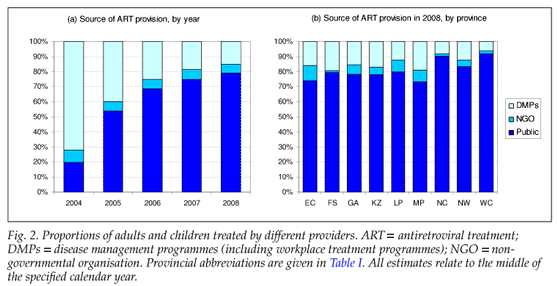
By the middle of 2008, an estimated 568 000 adults and children were receiving antiretroviral treatment in South Africa, which is more than twice the number 2 years previously, and more than 10 times the number at the middle of 2004 (Table I). Although 72% of patients in 2004 were receiving treatment through DMPs or WPTPs, this proportion declined to 15% by mid-2008, following the rapid scaling up of antiretroviral access in the public health sector (Fig. 2a). The proportion receiving treatment through NGO programmes has remained stable at around 6%, though this figure varies substantially between the provinces (Fig. 2b).
Over the years 2000 - 2008, the estimated CD4 distribution of the HIV-infected adult population changed substantially (Fig. 3a). The proportion of infected adults who have a CD4+ count >350/µl and are not on treatment has decreased from 70% in 2000 to 54% in 2008, and the proportion of infected adults in need of treatment, by current DoH eligibility criteria, has increased from 13% to 25% over this period. However, the proportion of infected adults who have CD4+ counts >350/µl and are not on treatment was relatively uniform across the provinces in 2008, at between 53% and 57% (Fig. 3b).
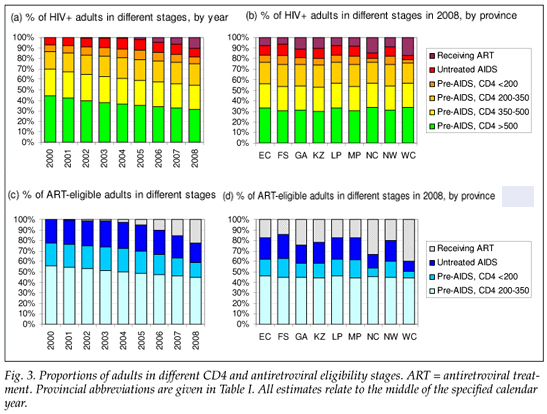
Antiretroviral coverage in adults has improved substantially, rising from 4.9% in 2004 to 40.2% in 2008, according to DoH eligibility criteria (Table II). Estimates of coverage change substantially when different definitions of treatment eligibility are used; when 'unmet need' is defined only as untreated AIDS, antiretroviral coverage in 2008 is estimated at 54.2%, but when 'unmet need' is defined according to the Southern African HIV Clinicians Society guidelines, coverage is estimated at only 22.2% (Fig. 3c). Adult antiretroviral coverage also varies greatly between provinces, ranging from 25.8% in the Free State to 71.7% in the Western Cape in 2008. Similar variability is observed when using the HIV Clinicians Society guidelines to define unmet need (Fig. 3d).
The total number of untreated adults needing antiretroviral treatment, at the middle of 2008, is estimated to be around 760 000 using the DoH eligibility criteria, 430 000 using the AIDS sick criterion, and 1.79 million using the HIV Clinicians Society criteria (Table III). These estimates of unmet need are relatively insensitive to changes in the assumed rates of retention on antiretroviral treatment and the assumed proportion of those starting treatment who have already progressed to AIDS. However, the estimates are very sensitive to the uncertainty regarding the annual numbers of new HIV infections in South Africa; the estimated total number of untreated adults who are sick with AIDS or have a CD4+ count <200/µl changes to 480 000 and 1.01 million when the lower and upper estimates of the annual new adult HIV infections are substituted into the model. The estimates of unmet need are also quite sensitive to the choice of HIV progression parameters. Using the progression parameters estimated by Hendriks et al.19 for men in Amsterdam over the 1985 - 1990 period, the unmet need reduces to 600 000, but using the progression parameters estimated by Longini et al.21 for USA military personnel, the unmet need increases to 990 000.
Discussion
This study demonstrates significant progress in the provision of antiretroviral treatment in South Africa, particularly after the phasing in of antiretroviral treatment in the public health sector after 2003. However, a large unmet need for antiretroviral treatment remains and, by the middle of 2008, only 40.2% of adults needing antiretroviral treatment were receiving it. A significant barrier to the expansion of the antiretroviral treatment programme is the limited number of public health facilities providing treatment and their shortage of health workers. An urgent need therefore exists for greater decentralisation of antiretroviral treatment services32 and greater recruitment and retention of health workers in the public health sector.33-36 A further barrier to improving antiretroviral coverage is the high proportion of eligible individuals who are unaware of their HIV status; in the 2005 HSRC household survey, for example, only 36% of HIV-infected adults had ever been tested for HIV.37 Stigma and confusion regarding the efficacy of antiretroviral treatment relative to traditional medicines are also significant factors inhibiting access to antiretroviral treatment;32 leaders at all levels must present clear and consistent messages to overcome these barriers.
Our analysis also demonstrates significant inequality in access to antiretroviral treatment in South Africa, with coverage in mid-2008 ranging from 25.8% in the Free State to 71.7% in the Western Cape. This appears to be mostly owing to variability in the performance of the public health sector, since the provinces with the highest coverage (Western Cape and Northern Cape) have the highest proportions of patients managed in the public sector, and the provinces with low coverage (Free State, Eastern Cape, Mpumalanga and Limpopo) have low proportions of patients managed in the public sector. The high coverage in the Western Cape and Northern Cape could also reflect their relatively low HIV prevalence.
We present a novel approach to estimating the unmet need for antiretroviral treatment. Although it is possible to conduct surveys to measure the unmet need for treatment at a given time,25, 38 this analysis shows that the CD4 distribution in the HIV-infected population can be expected to change substantially over time. Since it is costly to conduct surveys, mathematical models provide a simple alternative method for estimating the change in the unmet need for treatment as the epidemic progresses. The Spectrum model employed by UNAIDS, for example, estimates unmet need in adults by assuming that the CD4+ count in infected adults falls below the 350 and 200 thresholds at specified rates, based on CD4 data from Africa.39 The ASSA2003 model, which is commonly used in setting antiretroviral treatment targets in South Africa, quantifies unmet need in terms of WHO clinical staging,2 although this is a poor indication of unmet need according to combined CD4 and clinical criteria.38, 40-42 A mathematical model proposed by Williams et al.43 estimates unmet need based on local CD4 data, but does not incorporate clinical criteria. It would therefore appear that few mathematical models exist for estimating unmet need according to the combined clinical and CD4 criteria that are commonly used in defining antiretroviral eligibility. 4,6,7
Although our model has the advantage of quantifying unmet need in terms of various combinations of clinical and CD4 criteria, it is, like other models,3,44 parameterised using data that are not local to the setting in which the model is applied. Since distributions of CD4+ counts in HIV-negative adults and rates of CD4 decline in HIV-infected adults differ substantially between populations,43, 45 the HIV progression parameters that have been calculated from men in Amsterdam could be inappropriate for South Africa. We chose the progression parameters estimated from men in Amsterdam because they yielded the model results most consistent with South African data. For example, the model estimates of the proportion of untreated adults with CD4+ counts <200 (19%), 200 - 349 (20%), and 350 - 499 (25%) in 2004, are roughly consistent with the ranges measured in South African surveys between 2002 and 2005 (10 - 22%, 19 - 28% and 18 - 26% respectively).25-27 In addition, the median survival time estimated using the Amsterdam cohort data (10.8 years in the absence of highly active antiretroviral treatment) is roughly consistent with the median of 10.5 years estimated for South African gold miners aged 25 - 34 at the time of HIV acquisition23 and the median of 10.8 years estimated for adults aged 29 at the time of HIV acquisition, based on South African mortality data and HIV prevalence data.24 This suggests that the HIV progression parameters estimated from the Amsterdam cohort serve as a reasonable approximation to those in South Africa.
A potential concern is that data on the numbers starting treatment in the public sector could be subject to significant double-counting,8 and the rates of antiretroviral retention estimated from the Western Cape public health sector11 might not be applicable to other provinces. However, the estimates of numbers currently receiving antiretroviral treatment in the public health sector (Table I) are consistent with unpublished public sector drug distribution estimates produced by Aspen Pharmacare, which suggests that bias owing to double-counting and inter-provincial differences in antiretroviral retention is not substantial. Another limitation is the absence of data from some of the smaller DMPs and from individuals paying for their own treatment outside of DMPs,15 which may result in some under-estimation of antiretroviral coverage. Further work is needed to explore definitions of antiretroviral coverage other than the standard UNAIDS/UNGASS indicator, e.g. the proportion of newly eligible individuals in a given year who start treatment. Such measures may provide a more accurate indicator of recent programme performance, as they are not affected by the numbers of patients enrolled in the past. Further work is also required to produce separate estimates of antiretroviral coverage in men and women and to develop a separate model for estimating antiretroviral coverage in children.
We thank the many DMPs and NGOs that provided data from their programmes, and Andrew Boulle for providing helpful comments on an earlier version of this paper .
References
1. Statistics South Africa. Mortality and causes of death in South Africa, 2006: Findings from death notification . Pretoria: Statistics South Africa, 2008. http://www.statssa.gov.za (accessed 30 October 2008). [ Links ]
2. Johnson LF, Dorrington RE. Modelling the demographic impact of HIV/AIDS in South Africa and the likely impact of interventions. Demographic Research 2006; 14: 541-574. [ Links ]
3. Walensky RP, Wood R, Weinstein MC, et al. Scaling up antiretroviral therapy in South Africa: the impact of speed on survival. J Infect Dis 2008; 197(9): 1324-1332. [ Links ]
4. Department of Health. Operational Plan for Comprehensive HIV and AIDS Care, Management and Treatment for South Africa . Pretoria: Department of Health, 2003. www.info.gov.za/otherdocs/2003/aidsplan.pdf (accessed 28 November 2003). [ Links ]
5. Dorrington RE, Johnson LF, Bradshaw D, Daniel T. The Demographic Impact of HIV/AIDS in South Africa. National and Provincial Indicators for 2006 . Cape Town: Centre for Actuarial Research, South African Medical Research Council and Actuarial Society of South Africa, 2006. http://www.commerce.uct.ac.za/care (accessed 6 Dec 2006). [ Links ]
6. World Health Organization. Scaling Up Antiretroviral Therapy in Resource-Limited Settings: Treatment Guidelines for a Public Health Approach (2003 revision) . Geneva: WHO, 2004. http://www.who.int/hiv/pub/prev_care/en/arvrevision2003en.pdf (accessed 13 September 2004). [ Links ]
7. Southern African HIV Clinicians Society. Antiretroviral therapy in adults. South African Journal of HIV Medicine 2008; 9(1): 18-31. [ Links ]
8. Boerma JT, Stanecki KA, Newell ML, et al. Monitoring the scale-up of antiretroviral therapy programmes: methods to estimate coverage. Bull WHO 2006; 84(2): 145-50. [ Links ]
9. UNAIDS. 2008 Report on the Global AIDS Epidemic . Geneva: WHO, 2008. [ Links ]
10. Department of Health. National Comprehensive HIV and AIDS Plan Statistics; 2006 . Available: http://www.doh.gov.za/docs/statistics-f.html (accessed 1 December 2006). [ Links ]
11. Boulle A, Bock P, Osler M, et al. Antiretroviral therapy and early mortality in South Africa. Bull WHO 2008; 86(9): 678-687. [ Links ]
12. Regensberg LD, Hislop MS. A report back on more than four years of HIV/AIDS disease management in southern Africa. South African Journal of HIV Medicine 2003; 4(1): 7-10. [ Links ]
13. Stein A, McLeod H, Achmat Z. The Cover Provided for HIV/AIDS Benefits in Medical Schemes in 2002 . Cape Town: Centre for Actuarial Research, University of Cape Town, 2002. [ Links ]
14. Poole C, Stewart R. Public Sector HAART Projects - a Summary Report . Durban: Health Systems Trust, 2004. [ Links ]
15. Johnson LF, McLeod HD. Steady growth in antiretroviral treatment provision by disease management and community treatment programmes. S Afr Med J 2007; 97(5): 358-359. [ Links ]
16. Nachega JB, Hislop M, Dowdy DW, et al. Adherence to highly active antiretroviral therapy assessed by pharmacy claims predicts survival in HIV-infected South African adults. J Acquir Immun Defic Syndr 2006; 43(1): 78-84. [ Links ]
17. Charalambous S, Innes C, Muirhead D, et al. Evaluation of a workplace HIV treatment programme in South Africa. AIDS 2007; 21 (Suppl 3): S73-78. [ Links ]
18. Department of Health. South Africa Demographic and Health Survey 2003: Preliminary Report . Pretoria: Department of Health, 2004. http://www.doh.gov.za/docs (accessed 12 November 2008). [ Links ]
19. Hendriks JC, Craib KJ, Veugelers PJ, et al. Secular trends in the survival of HIV-infected homosexual men in Amsterdam and Vancouver estimated from a death-included CD4-staged Markov model. Int J Epidemiol 2000; 29(3):565-72. [ Links ]
20. Hendriks JC, Satten GA, Longini IM, et al. Use of immunological markers and continuous-time Markov models to estimate progression of HIV infection in homosexual men. AIDS 1996; 10(6): 649-656. [ Links ]
21. Longini IM, Clark WS, Gardner LI, Brundage JF. The dynamics of CD4+ T-lymphocyte decline in HIV-infected individuals: a Markov modeling approach. J Acquir Immun Defic Syndr 1991; 4(11): 1141-1147. [ Links ]
22. Satten GA, Longini IM. Markov chains with measurement error: estimating the 'true' course of a marker of the progression of human immunodeficiency virus disease. Appl Statist 1996; 45(3): 275-309. [ Links ]
23. Glynn JR, Sonnenberg P, Nelson G, Bester A, Shearer S, Murray J. Survival from HIV-1 seroconversion in Southern Africa: a retrospective cohort study in nearly 2000 gold-miners over 10 years of follow-up. AIDS 2007; 21(5): 625-632. [ Links ]
24. Johnson LF, Dorrington RE, Matthews AP. An investigation into the extent of uncertainty surrounding estimates of the impact of HIV/AIDS in South Africa. S Afr J Sci 2007; 103: 135-140. [ Links ]
25. Auvert B, Males S, Puren A, Taljaard D, Carael M, Williams B. Can highly active antiretroviral therapy reduce the spread of HIV? A study in a township of South Africa. J Acquir Immun Defic Syndr 2004; 36(1): 613-621. [ Links ]
26. Connelly D, Veriava Y, Roberts S, et al. Prevalence of HIV infection and median CD4 counts among health care workers in South Africa. S Afr Med J 2007; 97(2): 115-120. [ Links ]
27. Rehle T, Shisana O. The Impact of Antiretroviral Treatment on AIDS Mortality: A Study Focusing on Educators in South African Public Schools . Cape Town: Human Sciences Research Council and Medical Research Council, 2005. [ Links ]
28. Bekker LG, Myer L, Orrell C, Lawn S, Wood R. Rapid scale-up of a community-based HIV treatment service: programme performance over 3 consecutive years in Guguletu, South Africa. S Afr Med J 2006; 96(4): 315-320. [ Links ]
29. Coetzee D, Hilderbrand K, Boulle A, et al. Outcomes after two years of providing antiretroviral treatment in Khayelitsha, South Africa. AIDS 2004; 18: 887-895. [ Links ]
30. Ford N, Reuter H, Bedelu M, Schneider H, Reuter H. Sustainability of long-term treatment in a rural district: the Lusikisiki model of decentralised HIV/AIDS care. South African Journal of HIV Medicine 2006; 7(4): 17-22. [ Links ]
31. Rosen S, Long L, Sanne I. The outcomes and outpatient costs of different models of antiretroviral treatment delivery in South Africa. Trop Med Int Health 2008; 13(8): 1005-1015. [ Links ]
32. Posse M, Meheus F, van Asten H, van der Ven A, Baltussen R. Barriers to access to antiretroviral treatment in developing countries: a review. Trop Med Int Health 2008; 13(7): 904-913. [ Links ]
33. Nattrass N. South Africa's "rollout" of highly active antiretroviral therapy: a critical assessment. J Acquir Immun Defic Syndr 2006; 43(5): 618-623. [ Links ]
34. Stewart R, Loveday M. Public HAART Projects in South Africa - Progress to November 2004 . Durban: Health Systems Trust, 2005. http://www.hst.org.za/uploads/files/haart_progress1104.pdf (accessed 10 June 2005). [ Links ]
35. Schneider H, Blaauw D, Gilson L, Chabikuli N, Goudge J. Health systems and access to antiretroviral drugs for HIV in Southern Africa: service delivery and human resources challenges. Reprod Health Matters 2006; 14(27): 12-23. [ Links ]
36. Bärnighausen T, Bloom DE, Humair S. Human resources for treating HIV/AIDS: needs, capacities, and gaps. AIDS Patient Care STDs 2007; 21(11): 799-812. [ Links ]
37. Shisana O, Rehle T, Simbayi LC, et al. South African National HIV Prevalence, HIV Incidence, Behaviours and Communication Survey, 2005 . Cape Town: HSRC Press, 2005. http://www.hsrcpress.ac.za (accessed 1 December 2005). [ Links ]
38. McGrath N, Kranzer K, Saul J, et al. Estimating the need for antiretroviral treatment and an assessment of a simplified HIV/AIDS case definition in rural Malawi. AIDS 2007; 21 (Suppl 6): S105-113. [ Links ]
39. Eligibility for ART in lower income countries collaboration. Duration from seroconversion to eligibility for antiretroviral therapy and from ART eligibility to death in adult HIV-infected patients from low- and middle-income countries: collaborative analysis of prospective studies. Sex Transm Infect 2008; 84 (Suppl i): i31-6. [ Links ]
40. Jaffar S, Birungi J, Grosskurth H, et al. Use of WHO clinical stage for assessing patient eligibility to antiretroviral therapy in a routine health service setting in Jinja, Uganda. AIDS Res Ther 2008; 5: 4. [ Links ]
41. Badri M, Bekker LG, Orrell C, Pitt J, Cilliers F, Wood R. Initiating highly active antiretroviral therapy in sub-Saharan Africa: an assessment of the revised World Health Organization scaling-up guidelines. AIDS 2004; 18(8): 1159-1168. [ Links ]
42. Kagaayi J, Makumbi F, Nakigozi G, et al. WHO HIV clinical staging or CD4 cell counts for antiretroviral therapy eligibility assessment? An evaluation in rural Rakai district, Uganda. AIDS 2007; 21(9): 1208-1210. [ Links ]
43. Williams BG, Korenromp EL, Gouws E, Schmid GP, Auvert B, Dye C. HIV infection, antiretroviral therapy, and CD4+ cell count distributions in African populations. J Infect Dis 2006; 194(10): 1450-1458. [ Links ]
44. Stover J, Johnson P, Zaba B, Zwahlen M, Dabis F, Ekpini RE. The Spectrum projection package: improvements in estimating mortality, ART needs, PMTCT impact and uncertainty bounds. Sex Transm Infect 2008; 84 (Suppl i): i24-30. [ Links ]
45. Williams BG, Dye C. Antiretroviral drugs for tuberculosis control in the era of HIV/AIDS. Science 2003; 301(5639): 1535-1537. [ Links ]
Accepted 11 May 2009.
* Corresponding author: L Johnson (Leigh.Johnson@uct.ac.za)













