Services on Demand
Journal
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Dental Journal
On-line version ISSN 0375-1562Print version ISSN 0011-8516
S. Afr. dent. j. vol.71 n.6 Johannesburg Jul. 2016
RADIOLOGY CASE
Maxillo-facial radiology case 142
CJ Nortjé
BChD, PhD, ABOMR, DSc. Faculty of Dentistry, University of the western Cape
A 6-year old boy presented to the hospital with a five- month history of a persistent, draining sore (Figs.1 & 2)) in the mandible on the left side. It all started when a carious 36 was extracted. Figs. 3, 4, 5 & 6 are images of other patients with the same condition. What is your diagnosis?



INTERPRETATION
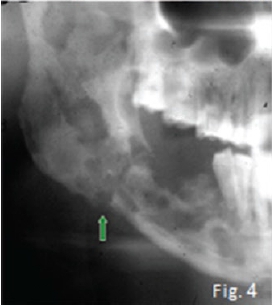
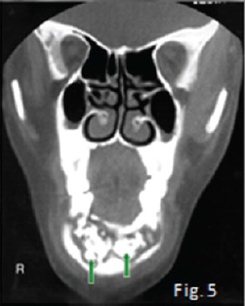
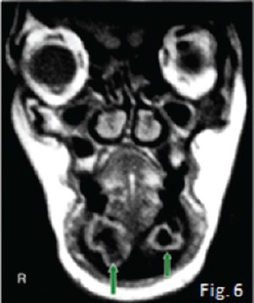
The cropped pantomograph (Fig 2) shows a "blurred/ fussy" appearance of the trabeculae due to loss of density. Signs of cortical destruction are also present. A provisional diagnosis of acute osteomyelitis was made which was confirmed histologically. Osteomyelitis is an inflammation of bone cortex and marrow that develops in the jaw usually after a chronic infection: No detectable radiographic features of the infection are discernible in the first 8-10 days (radiological principle: 30-60% decalcification before any changes are observed). About three weeks after the start of the infection irregular radiolucencies with enlargement of trabecular spaces are noticed (Fig 3). In the chronic stages, extensive areas of the bone may be destroyed and sequestra are formed showing the classic moth-eaten appearance and occasionally a pathological fracture may also be present (Fig. 4). Note the sequestration of bone in the anterior mandible on the coronal CT scan (Fig. 5) of another patient with chronic suppurative osteomyelitis The coronal T2 W. MRI scan (Fig. 6) shows the sequestrated bone (no signal black) is surrounded by zones of high signal intensity (white signal) representing the regions of active inflammation. Most cases of osteomyelitis of the jaw result from odontogenic infections, infections from a fracture site; or, rarely, haematogenous spread from a distant site, which is more common in the long bones. The cause of infection is most frequently Staphylococcus aureus, but haemolytic streptococci and Bacteroides are also encountered. The mandible is by far the most frequently affected; the adult maxilla is very seldom the site of osteomyelitis. The acute phase of suppurative osteomyelitis is sudden in onset and rapid in course. The patient experiences severe pain, fever, regional lymphadenopathy, and leucocytosis. Teeth in the region become loose and tender to percussion. When the mandible is involved there may be paraesthesia of the lower lip on the affected side. As soon as drainage is established, the pain eases, the temperature drops, the patient becomes more comfortable. Without treatment the infection may progress into a protracted chronic suppurative osteomyelitis. Differential diagnoses include malignancies and oteoradionecrosis.
Reference
1. Farman AG, Nortje CJ & Wood R E: Oral and Maxillofacial Imaging, 1st Ed, Mosby. St. Louis, Missouri 1993 pp. 191-195 [ Links ]
 Correspondence:
Correspondence:
CJ Nortjé
E-mail: cnortje@uwc.ac.za













