Serviços Personalizados
Journal
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
Southern African Journal of Critical Care (Online)
versão On-line ISSN 2078-676Xversão impressa ISSN 1562-8264
South. Afr. j. crit. care (Online) vol.40 no.1 Pretoria Mar. 2024
https://doi.org/10.7196/SAJCC.2024.v40i1.1141
RESEARCH
Bedside critical care training: A quasi-experimental study in the paediatric emergency department of a referral hospital in Nigeria
M T AbiodunI, II; E A OchabaIII; A Kpongo-OgievaIII
IMB BS, MPH, FWACP (Paed); Paediatric Emergency Division, Department of Child Health, University of Benin Teaching Hospital, Benin City, Edo State, Nigeria
IIMB BS, MPH, FWACP (Paed); Department of Child Health, School of Medicine, College of Medical Sciences, University of Benin, Benin City, Edo State, Nigeria
IIIMB BS, MWACP; Paediatric Emergency Division, Department of Child Health, University of Benin Teaching Hospital, Benin City, Edo State, Nigeria
ABSTRACT
BACKGROUND. There is a need for critical care services outside intensive care units (ICUs), especially in emergency departments (EDs). However, there is a paucity of skilled manpower for ED critical care or emergency critical care (ECC) in resource-limited settings.
OBJECTIVE. To evaluate the impact of bedside training on emergency critical care practices of clinical staff.
METHODS. This was a quasi-experimental study using a pretest - post-test design in a paediatric ED. The intervention was a six-week structured bedside training on bubble continuous positive airway pressure (CPAP) high-flow nasal cannula (HFNC) and mechanical ventilation. Participants' actual ECC practices pre and post training were evaluated, including their perceived proficiency on an uncalibrated 100 mm visual analogue scale (VAS). Descriptive and inferential analyses were done; p<0.05 was considered significant.
RESULTS. A total of 35 clinical staff participated in the training, comprising 9 (24.3%) paediatric registrars, 12 (32.5%) senior registrars, 10 (27.0%) nurses, 4 (10.8%) house officers and 2 (5.4%) paediatric consultants. The male: female ratio of the participants was 1:1.6, and their mean (SD) age was 33.24 (6.30 years. Participants' understanding of testing the CPAP circuit, connecting the patient and weaning significantly improved following training (p=0.004). Their capacity to select appropriate HFNC parameters improved (p=0.013). They performed more endotracheal intubations in the post-training period (p=0.001). Their pretest-post-test proficiency in mechanical ventilation increased on VAS (mean scores 45.26+31.99 v. 63.26+22.26; p=0.038). Also, there was a significant increase in their perceived proficiency in paediatric analgesia/sedation (30.83+29.86 v. 49.83+23.90; p=0.029.
CONCLUSION. Short-term bedside critical care training enhanced the self-reported competency of paediatric ED staff. There is a need for on-the-job ECC training and retraining of clinical staff in our setting.
Keywords: Emergency critical care, children, bedside training, clinical staff.
Paediatric critical care (PCC) or intensive care is an evolving medical subspecialty especially in low- and middle-income countries (LMICs).[1] PCC requires highly skilled clinical staff including paediatric intensivists, nurses, visiting subspecialists and surgeons as well as other members of the medical team to carry out multidisciplinary management of patients with life-threatening illnesses by supporting organ functions and averting further deterioration. Although intensive care unit (ICU) services can reduce mortality of acutely ill children often encountered in resource-limited settings, ICU bed spaces are often in short supply.[2,3] There is a need for provision of critical care services outside the four walls of ICUs, especially in acute care areas.[4,5] Emergency department critical care or emergency critical care (ECC) service is an attempt to bridge this gap. It enables prompt delivery of relevant critical care to acutely ill children before an ICU transfer.[6,7] ECC has the potential to enhance the monitoring, treatment and outcome of critically ill children especially in health facilities running mixed ICUs with limited paediatric bedspaces.[5,7] In addition, the prohibitive cost of ICU admissions is often unaffordable to many patients in this environment, which often results in undue delays of admission into ICU even when bed spaces are available. This delay highlights the need for provision of short-term critical care services outside the enclave of ICUs, considering that healthcare delivery is predominantly by out-of-pocket spending in the sub-region.[8,9] Hence, emergency department (ED) critical care is pertinent to promptly optimising the care of acutely ill children.
However, there are limited ECC training opportunities for clinical staff in paediatric EDs because critical care is not a major part of paediatric training curricula at present.[10,11] This is undesirable because significant proportions of children being managed by paediatric practitioners in the sub-region are critically ill.[3] This limited staff exposure to critical care training as well as inadequate physical resources obviously worsen the outcomes of severe childhood illnesses in our setting.[3,12] While efforts are being made to avert late presentation of children to health facilities, there is a need to improve specialised healthcare delivery at paediatric EDs.[3,11] This will ensure early and optimal management of an acutely ill child before ICU admission is achieved, if unavoidably required.[13] Canarie et al. highlighted the dearth of paediatric critical care skills in our medically-underserved region.[14] Bjorklund et al. opined that collaboration in the exchange of skills is essential to promote pediatric critical care in our sub-region.[15] In a recent nation-wide survey, Enyuma et al. found that a majority of medical and nursing staff in paediatric EDs in Nigeria have not completed relevant subspecialty training.[16] Likewise, Abiodun et al. found that less than a fifth of paediatric trainees in Nigeria had certification in a paediatric advanced life support (PALS) course.[3] This can undermine ECC preparedness and worsen the prevalent poor health indices in this setting.
Considering the foregoing and the ongoing strategic upgrading of critical care facilities in our centre, there is a need to build the ECC capacity of our frontline clinical staff. Hence, regular on-the-job training in critical care for clinicians in our paediatric ED is timely. The present study aims to evaluate the impact of structured bedside training on the staff's understanding and skills in invasive/non-invasive ventilation at our Children's Emergency Room (CHER). We hypothesise that this up-skilling training will enhance the clinical knowledge and ECC practice of medical staff in theCHER.
Methods
Study setting and participants
This study took place at the Critical Care Bay of the CHER of the University of Benin Teaching Hospital (UBTH) in southern Nigeria. The study period was from May to July 2022. Multiparameter monitors, an automated external defibrillator (AED), bubble continuous positive airway pressure (CPAP) devices, high-flow nasal cannula (HFNC) oxygen delivery systems (Airvo2; Fisher & Paykel) and Siaree paediatric ventilators (Siaretron 2000 and Falco 202 EVO) were available in the critical care bay. Also, there were manikins for simulation.
Participants were clinical staff/trainees working or taking calls in the CHER who were mainly house officers, nurses and paediatric residents. Visiting clinicians and paramedic students were excluded.
Study design
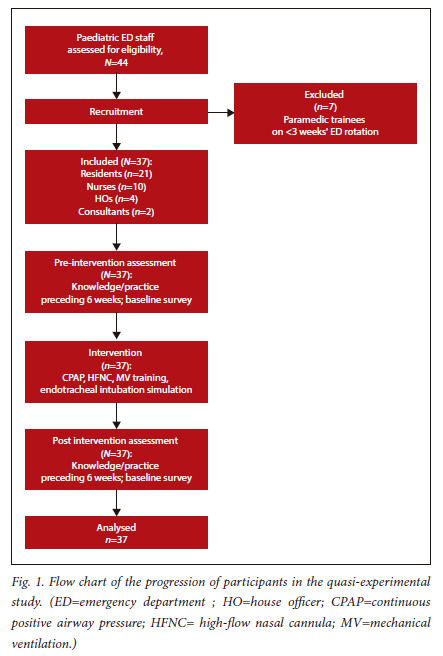
This was a prospective quasi-experimental study using a pre- and post-test design as depicted below (Fig. 1).
Pre-test
A pretested feedback form was administered to every participant in the study in the pre-intervention period to document their knowledge and self-reported practice of respiratory support (CPAP, HFNC and mechanical ventilation) 6 weeks prior to the training. This form described their baseline scope of practice and skills.
Interventions
The intervention comprised structured bedside training sessions on critical care equipment and case-based discussions (CBDs) over a 6-week period (May/June 2022). The equipment used in the training included CPAP, Airvo2 and Siaree mechanical ventilators. The participants were scheduled in groups of 8 - 10 for bedside clinical instructions and 2 - 4 persons for hands-on practice sessions: 1 hour on Thursdays (08h00 - 09h00) and 30 minutes thrice weekly during hand-over afternoon rounds. Components of the bedside training include setting up of the equipment, selection of appropriate patient interfaces, selection of appropriate modes and ventilation parameters, adjustment of ventilator settings, interpretation of ventilator waveforms, trouble-shooting, and weaning procedures. Participants focused on their scope of practice during training. AED use and endotracheal intubation were simulated on low-fidelity manikins that were available in the unit and the departmental simulation laboratory. Case-based discussions were virtually done using de-identified patient information and clinical scenarios. In addition, flexible self-learning was encouraged among participants during the period guided by the unit's standardised ECC checklists on invasive and non-invasive ventilation as well as manufacturers' instructional videos for quality assurance.[17,18]
Post test
The feedback form was again administered to participants to document their knowledge and self-reported practice of respiratory support using CPAP, HFNC and mechanical ventilation (MV) in the 6-week period after completion of training. Participants' overall proficiency was assessed on a 100 mm uncalibrated visual analogue scale (VAS).
Sample size
This was a total population study of all consenting clinical staff working or taking call duties at the paediatric emergency department during the five-month study period. Participants were purposively recruited.
Data collection
This was done using a feedback form comprising sections on each participant's baseline information, perception of bedside ECC training, perceived ECC proficiency, self-reported ECC practice and perceived challenges/recommendation. The preliminary form was pretested and found satisfactory among paediatric staff who attended the maiden ECC didactic teaching at the department of child health seminar room in 2021. The feedback form was administered twice to every participant: as a pretest and a post-test.
Data analysis
The data were analysed using SPSS version 26.0 statistical software for Windows (IBM, USA). Fisher's exact test or the chi-square was used to compare categorical data such as gender and type of institution. A weighted mean score was computed for variables on each sub-scale. Adequate perception was defined with a cut-off point of 2.5 on a 4-point Likert scale. Self-reported ECC practices pre and post training were evaluated, including proficiency on an uncalibrated 100 mm visual analogue scale (VAS). VAS scores >50 were rated as adequate, while scores >70 were considered excellent. The F-test (or Student's t-test where appropriate) was used to detect significant differences among weighted mean scores while Scheffé's post hoc test identified significantly different weighted mean scores on the F-test. p<0.05 was considered significant.
Ethical consideration
Participation was entirely voluntary; names and identifying numbers were not required. Ethical clearance for the study was obtained from the Ethics and Research Committee of the College of Medical Sciences, University of Benin (ref. no. CMS/REC/2023/344).
Results
Baseline characteristics of participants
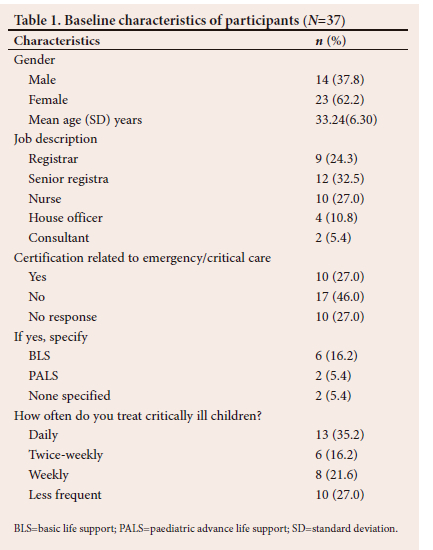
A total of 37 clinical staff took part in the beside training, comprising 9 (24.3%) paediatric registrars, 12 (32.5%) senior registrars, 10 (27.0%) nurses, 4 (10.8%) house officers and 2 (5.4%) paediatric consultants (Table 1). The male:female ratio of the participants was 1:1.6, and their mean (SD) age was 33.24 (6.30) years. Six (16.2%) participants stated that they had certification in basic life support while 2 (5.4%) were certified in paediatric advanced life support. Thirteen (35.1%) participants indicated that they daily attended to critically ill children in their units; other details are in Table 1. Seven paramedic students took part in the baseline survey but were excluded from all analysis because they could not complete the training owing to a change in their clinical rotation from the emergency unit.
Participants' perception of bedside training and perceived ECC proficiency
Table 2 shows participants' agreement levels with statements on ECC bedside training. They fully agreed that it was relevant to their clinical practice and career. Their pre- and post-test results in perceived proficiency in paediatric mechanical ventilation improved significantly on an uncalibrated 100 mm visual analogue scale (VAS) (45.26+31.99 v. 63.26 (22.26); p=0.038). Also, there was a significant increase in their perceived proficiency in paediatric analgesia/sedation on the VAS (30.83 (29.86) v. 49.83 (23.90); p=0.029). On sub-analysis, doctors' perceived proficiency in invasive ventilation significantly increased post training (35.36 (23.24) v. 63.26 (22.26); p=0.001); likewise, nurses showed improved proficiency in non-invasive ventilation post training (p=0.02).
There was no baseline variable that independently predicted a VAS score >70 among participants (p=0.08).
Effects of bedside training on participants' actual ECC practice
There was improved adherence to the unit checklist on choice of ventilator settings by participants in the post-training period. Table 3 shows the self-reported ECC practice of participants in the 6-week periods before and after training. They recognised significantly more children requiring endotracheal intubation in the post-training period (p=0.002) and they intubated more children during the period (p=0.001). Reasons given by participants for failure to intubate in the post-training period were inappropriate size of laryngoscope blade (n=3 (8.1%)), malfunctioning laryngoscope (n=3 (8.1%)) and absence of a free ventilator (n=2 (5.4%))
Participants' proficiency on ECC equipment and interfaces
Table 4a shows the effect of bedside training on participants' proficiency in using the CPAP device, HFNC device (Airvo2, Fisher and Paykel) and Siaree ventilators (Sietron 2000 and Falcom 500). Participants' understanding of testing the CPAP circuit, connecting to the patient and weaning significantly improved following training (p=0.004). Likewise, their capacity to select appropriate Airvo2 parameters improved (p=0.013) and there was a significant increase in their competence in all aspects of paediatric invasive ventilation (p<0.05; Table 4a).
Overall, participants' aggregate understanding of each of the three types of respiratory support equipment significantly improved following training, (p<0.05). At baseline, their understanding of invasive ventilation was much less than their competency in non-invasive ventilatory supports (CPAP and Airvo2) as shown in Table 4b (F=8.287; p=0.001). However, post training, their perceived competency in invasive respiratory support improved, comparable to their competency in non-invasive supports (F=1.949; p=0.155).
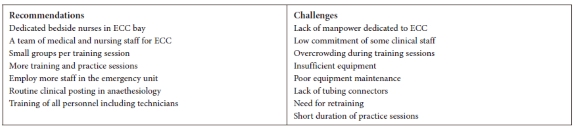
Challenges to ECC beside training and recommendations by participants
The challenges and recommendations for ECC bedside training given by participants are listed below, following thematic analysis (Box 1). Pre- and post-training lists of perceived challenges (X2=30.440; df=21; p=0.83) and recommendations for improvement (X2=42.444; df=31; p=0.83) by participants were similar.
Discussion
The present study suggests that short-term bedside training has a beneficial influence on the critical care proficiency of clinical staff in a CHER, as is evidenced by the significant increase in their perceived competence in ECC practice; this finding is comparable to earlier reports by Asani et al. in Lagos, and Abiodun et al. in Benin City, that bedside training improved the clinical competency of undergraduate trainees.[19,20] Also, bedside teaching in the emergency department has been found to be useful in delivering effective learner-centered feedback.[21] Over half of our participants expressed satisfaction with the training objectives and agreed that bedside training will enhance their future professional development. On-the-job and off-the-job training opportunities have been linked to job satisfaction and career development of health professionals. Lasebikan et al. in Enugu IN south-east Nigeria found that health workers expressed low job satisfaction when they had limited opportunity for professional training in their careerS.[22] This is consistent with findings in other parts of the country and elsewhere on the continent.[23,24]
Furthermore, the actual number of successful critical care procedures including endotracheal intubation performed by the participants increased post-training comparable to the report by Al-Wassia et al. in Saudi Arabia that simulation-based training resulted in sustained improvement in paediatric residents' intubation skills.[25] Based on the National Emergency Airway Registry for Neonates in the USA, Johnston et al. similarly found that higher clinical experience was associated with an increased first-attempt success rate of endotracheal intubation by physicians.[26] This highlights the need to incorporate regular skill acquisition drills into emergency and critical care training in all settings in order to achieve improved access to safer paediatric procedures. Regular training of clinical staff can be life-saving in our medically-underserved region where delayed presentation and sub-optimal interventions in health facilities contribute to poor outcome of paediatric emergencies.[27,28] Nonetheless, our participants desired the opportunity to undergo long-term critical care training including clinical rotations in intensive care units which has been found to be beneficial to paediatric residents in other settings.[29,30]
Participants' baseline understanding of respiratory support equipment and patient interfaces was low, consistent with earlier reports of shortages of critical care resources in (LMICs.[31,32] Moreover, the limited availability of PCC equipment in our setting obviously contributed to the limited baseline competency and understanding of such devices among our participants, as previously found by Abiodun et al. among paediatric trainees in Nigeria.[3] Our participants' insight into invasive ventilation was particularly low, perhaps because of the chronic dependence on adult intensivists in mixed intensive care units to manage children in the setting.[2,3] However, there was a significant increase in understanding of the principles and usage of bubble CPAP devices, HFNC oxygen delivery systems and invasive mechanical ventilation among our participants post training, highlighting the benefits of training and retraining of staff on medical devices in clinical practice.[14,18]
Sustaining the acquired skills on the use of critical care equipment and accessories in resource-limited setting demands a good maintenance culture to keep devices functional at all times.[17] Our participants reported an improvement in their capacity to sterilise tubing and devices when necessary as well as trouble-shoot for possible causes of desaturation in a child being ventilated. Nonetheless, competent biomedical engineering services are needed for prompt equipment repair, especially in developing settings with the limited quantity of respiratory support equipment available in our health facilities.[3,33] Unfortunately, biomedical repair services are often not readily available, worsening the shortage of functional equipment, especially in rural health facilities in the sub-region.[33]
Challenges identified by our participants that hinder ECC training include limited physical resources and dedicated manpower, similar to earlier reports by Abiodun et al. and Canarie et al. that LMICs have limited human and physical resources for paediatric critical care in spite of their high burden of critical childhood illnesses.[3,14] Collaboration and local innovation can partly bridge these gaps.[15] Also, participants recommended more hands-on practice opportunities as well as ICU clinical rotations. Consequent to participant feedback on this step-down training, a CHER-ICU posting has been commenced for paediatric senior registrars at the study centre. Poor healthcare financing was stated as a challenge that can be addressed by increased government commitment to ECC service delivery and improved health insurance coverage for children in the populace; this will mitigate the catastrophic effects of healthcare spending on households.
The strength of the present study includes the involvement of different cadres of clinical staff in bedside training. Also, real-life equipment and patient interfaces were used for training; this enables participants to acquire relevant skills in the practice of non-invasive and invasive ventilation as well as becoming familiar with those specific devices. Such device-specific proficiency cannot be readily acquired via online simulation modules, despite their effectiveness as immersive learning tools. Nonetheless, a limitation of this study is that trainees' proficiency levels were based on their self-reported feedback rather than onsite assessments of trainees' performances by the trainers or independent external assessors. Self-reporting could predispose to a recall bias. Moreover, a small sample size limited the extent of sub-analysis of the study sub-groups.
Conclusion and recommendations
Bedside paediatric critical care training enhances the perceived competency of emergency department staff in performing invasive and non-invasive ventilation. There is a need for regular on-the-job emergency critical care training and retraining of clinical staff in the setting as well as elective ICU posting for paediatric registrars. Also, a large multi-centre study focusing on the effects of bedside training on paediatric critical care is desirable in the country.
Declaration. This study was presented in January 2023 at the Paediatric Association of Nigeria Conference (PANCONF) in Akure, Ondo State, south-west Nigeria.
Acknowledgements. This study was a part of step-down trainings of a Commonwealth medical fellowship in paediatric intensive care (undergone by the lead researcher). Development of the ECC checklists used in this study was also part of his post-fellowship activities. The authors thank paediatric chief residents at the institution.
Author contributions. MTA conceptualised the study, wrote the protocol and facilitated the training. EAO and AKO co-facilitated the training and collected/interpreted research data. EAO carried out a prior presentation (see declaration above). MTA wrote the initial draft of the manuscript. All authors critically reviewed and approved the final manuscript.
Funding. The authors received no financial support for the research, authorship and/or publication of this article.
Conflicts of interest. None.
References
1. Turner EL, Nielsen KR, Jamal S, von-Saint Andre-von Arnim A, Musa NL. A review of pediatric critical care in resource limited settings: A look at past, present and future directions. Front Pediatr 2016;4:5. https://doi.org/10.3389/fped.2016.00005 [ Links ]
2. Akindolire AE, Tongo OO. Paediatric critical care needs assessment in a tertiary facility in a developing country. Niger J Paediatr 2018;45(1):10-14. https://doi.org/10.4314/njp.v45i1.3 [ Links ]
3. Abiodun MT, Eki-Udoko FE. Evaluation of paediatric critical care needs and practice in Nigeria: Paediatric residents' perspective. Crit Care Res Pract 2021:2000140. https://doi.org/10.1155/2021/2000140 [ Links ]
4. Hillman K. Critical care without walls. Curr Opin Crit Care 2002;8(6):594-599. https://doi.org/10.1097/00075198-200212000-00019 [ Links ]
5. Silva AC, Oyama CB, Grion CM, et al. Caring for critically ill patients outside ICUs due to a full unit. Crit Care 2015 (Suppl 2):19. https://doi.org/10.1186/cc14673 [ Links ]
6. Burke TF, Hines R, Ahn R, et al. Emergency and urgent care capacity in a resource-limited setting: An assessment of health facilities in Western Kenya. BMJ Open 2014;4:e006132. [ Links ]
7. Murthy S, Sayeed SA, Adhikari NKJ. (2014) Critical care in low-resource settings. In: Scales D, Rubenfeld G, editors. The Organisation of Critical Care. Respiratory Medicine, vol. 18. Humana Press, New York. https://doi.org./10.1007/978-1-4939-0811-0_16 [ Links ]
8. Onoka CA, Hanson K, Hanefeld J. Towards universal coverage: A policy analysis of the development of the National Health Insurance Scheme in Nigeria. Health Policy Plan 2015;30(9):1105-1117. https://doi.org/10.1093/heapol/czu116 [ Links ]
9. Ibukun C, Komolafe E. Household catastrophic health expenditure: Evidence from Nigeria. Microeconomics and Macroeconomics 2018;6(1):1-8. https://doi.org/10.5923/j.m2economics.20180601.01 [ Links ]
10. National Paediatric Subspecialty Curriculum. https://npmcn.edu.ng/paediatrics-curriculum-and-logbook/ (accessed 8 December 2022). [ Links ]
11. Fant CD, Schwartz KR, Patel H, et al. Developing and implementing a pediatric emergency care curriculum for providers at district level hospitals in Sub-Saharan Africa: A case study in Kenya. Front Public Health 2017;5:322. https://doi.org/10.3389/fpubh.2017.00322 [ Links ]
12. Ibrahim A, Scruth E, Adeyinka A, et al. Development of paediatric critical care in northwestern Nigeria: Initial implementation with a needs assessment model. Aust Crit Care 2022;35(3):279-285. https://doi.org/10.1016/j.aucc.2021.06.002 [ Links ]
13. Losonczy LI, Papali A, Kivlehan S, et al. White Paper on early critical care services in low resource settings. Ann Glob Health 2021;87(1):105. https://doi.org/10.5334/aogh.3377 [ Links ]
14. Canarie MF, Shenoi AN. Teaching the principles of pediatric critical care to non-intensivists in resource limited settings: Challenges and opportunities. Front Pediatr 2018;6:44. https://doi.org/10.3389/fped.2018.00044 [ Links ]
15. Bjorklund A, Slusher T, Day LT, et al. Pediatric critical care in resource limited settings - lessening the gap through ongoing collaboration, advancement in research and technological innovations. Front Pediatr 2022;9:791255. https://doi.org/10.3389/fped.2021.791255 [ Links ]
16. Enyuma COA, Moolla M, Motara F, Olorunfemi G, Geduld H, Laher AE. Paediatric emergency department preparedness in Nigeria: A prospective cross-sectional study. Afr J Emerg Med 2020;10(3):152-158. https://doi.org/10.1016/j.afjem.2020.05.010 [ Links ]
17. Quick Guide: Adding oxygen | Airvo 2 |. Auckland, NZ; Fisher & Paykel Healthcare. https://www.youtube.com/watch?v=vF5INHtJNio (accessed 20 April 2022). [ Links ]
18. AIRVO 2 High-Flow Standard Operating Procedure. https://www.clinicalguidelines.scot.nhs.uk/nhsggc-guidelines/nhsggc-guidelines/intensive-and-critical-care/airvo-2-high-flow-standard-operating-procedure (accessed 20 April 2022). [ Links ]
19. Asani M. Bedside teaching: An indispensable model of patient-centred teaching in undergraduate medical education. Niger J Basic Clin Sci 2014;11:57-61. [ Links ]
20. Abiodun MT, Ikhurionan PE. Clinical experience in children emergency room: A cross-sectional study of medical students at a university hospital in Nigeria. Nigerian J Paediatrics 2022;49(2):102-108. https://doi.org/10.4314/njp.v49i2.2 [ Links ]
21. Ryan M. Bedside teaching in the emergency department: A model for delivering effective learner-centered feedback. Creative Educ 2022;13:731-734. https://doi.org/10.4236/ce.2022.133046 [ Links ]
22. Lasebikan OA, Ede O, Lasebikan NN, Anyaehie UE, Oguzie GC, Chukwujindu ED. Job satisfaction among health professionals in a federal tertiary hospital in Nigeria. Niger J Clin Pract 2020;23(3):371-375. https://doi.org/10.4103/njcp.njcp_292_19 [ Links ]
23. Gyang MD, Dankyau M, Gidado S, Gyang BA, Madaki AJ. Job satisfaction among healthcare workers at a district hospital in Plateau State, Nigeria. J Med Trop 2018;20:111-116. [ Links ]
24. Merga H, Fufa T. Impacts of working environment and benefits packages on the health professionals' job satisfaction in selected public health facilities in eastern Ethiopia: Using principal component analysis. BMC Health Serv Res 2019;19(1):494. https://doi.org/10.1186/s12913-019-4317-5 [ Links ]
25. Al-Wassia H, Bamehriz M, Atta G, Saltah H, Arab A, Boker A. Effect of training using high-versus low-fidelity simulator mannequins on neonatal intubation skills of pediatric residents: A randomised controlled trial. BMC Med Educ 2022;22(1):497. https://doi.org/10.1186/s12909-022-03572-8 [ Links ]
26. Johnston L, Sawyer T, Ades A, et al. Impact of physician training level on neonatal tracheal intubation success rates and adverse events: A report from National Emergency Airway Registry for Neonates (NEAR4NEOS). Neonatology 2021;118(4):434-442. https://doi.org/10.1159/000516372 [ Links ]
27. Abiodun MT, Ilori OR. Caregivers' perception and determinants of delayed presentation of children with severe malaria in an emergency room in Benin City, Nigeria. Niger Postgrad Med J 2022;29(3):198-205. https://doi.org/10.4103/npmj.npmj_80_22 [ Links ]
28. Eze JN, Edelu BO, Ndu IK, Oguonu T. Paediatric emergency medicine practice in Nigeria: A narrative review. BMC Emerg Med 2023;23(1):31. https://doi.org/10.1186/s12873-023-00790-1 [ Links ]
29. Handley SC, Pouppirt N, Zucker E, Coughlin KA, Ades A. Improving the resident educational experience in a Level IV neonatal/infant intensive care unit. Pediatr Qual Saf 2020;5(6):e352. https://doi.org/10.1097/pq9.0000000000000352 [ Links ]
30. Tufts L, Worthy M, Putty K, et al. Improving resident experience during the pediatric intensive care unit rotation. Global Pediatrics 2023;3. https://doi.org/10.1016/j.gpeds.2022.100029 [ Links ]
31. Muttalib F, González-Dambrauskas S, Lee JH, et al. Pediatric emergency and critical care resources and infrastructure in resource-limited settings: A multicountry survey. Crit Care Med 2021;49(4):671-681. https://doi.org/10.1097/CCM.0000000000004769 [ Links ]
32. Abdelatif RG, Mohammed MM, Mahmoud RA, Bakheet MAM, Gima M, Nakagawa S. Characterisation and outcome of two pediatric intensive care units with different resources. Crit Care Res Pract 2020;Article ID 5171790, 6 pages. http://doi.org/10.1155/2020/5171790 [ Links ]
33. Thapa R, Yih A, Chauhan A, et al. Effect of deploying biomedical equipment technician on the functionality of medical equipment in the government hospitals of rural Nepal. Hum Resour Health 2022;20(1):21. https://doi.org/10.1186/s12960-022-00719-y [ Links ]
 Correspondence:
Correspondence:
M T Abiodun
moses.abiodun@uniben.edu
Accepted 21 January 2024
Contribution of the study
Paediatric emergency department clinical staff desire hands-on critical care training in developing settings. Bedside training improves the knowledge and skills of nursing staff in non-invasive ventilation. Bedside training also builds the capacity of medical staff in invasive ventilation in the emergency department. Overall, short-term bedside training enhances the clinical knowledge and self-reported critical care practice of clinical staff in Children's Emergency Room.













