Servicios Personalizados
Revista
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
Journal of Contemporary Management
versión On-line ISSN 1815-7440
JCMAN vol.11 no.1 Meyerton 2014
RESEARCH ARTICLES
Technology as a tool to develop a community health model
ED Meyer; S Stolz; S Smith
University of Pretoria
ABSTRACT
The paper describes a case study of a community health model that was developed and piloted at a University based clinic run in partnership with the South African Department of Health (DOH). The aim was to strategize, innovate and implement a collaborative care model strengthened by available technological resources that could improve the health and social outcomes of a struggling community.
The 5 C's e-Health framework for developing countries was applied to the case and compared to the Human Resources for Health 2030 strategy of Government to inform the development of a community care team (human capital based and enabled by an electronic management system) that could share patient health and social information, synergise resources and inform future community developments.
Key phrases: community health; electronic health system; national health insurance; primary healthcare; technological health developments
1. INTRODUCTION
"Health services systems have two main objectives: to maximise the health of a population and to minimize inequity or disparities of health amongst population groups" (Starfield 1998:3). In achieving its goal on better health for all, the World Health Organization (WHO) has identified five key elements of effective primary health care (World Health Organisation 2013:Internet).
■ universal coverage reforms: reducing exclusion and social disparities in health;
■ service delivery reforms: organizing health services around people's needs and expectations;
■ public policy reforms: integrating health into all sectors;
■ leadership reforms: pursuing collaborative models of policy;
■ dialogue: increasing stakeholder participation.
In 2010 the South African Minister of Health implemented the Revitalization of Primary Health Care initiative with the intent to address some of the challenges currently faced by the health sector. A policy paper (Department of Health 2011b:22-23) addressing challenges in the health care system in South Africa stated that primary health care services will be re-engineered "to focus on community outreach services ... which will be population orientated with extensive community outreach and home based services."
Primary health care services will be orientated towards proactive household and community focused interventions. It encompasses disease prevention, early detection and treatment of illness, community based disease management, rehabilitation and the promotion of healthy living. All this is underpinned by the acknowledgement that health and health care is a universal human right (Department of Health 2011b:23).
The Daspoort Clinic team acknowledged these challenges and established workgroups to pro-actively address them. The Daspoort Clinic provided a suitable environment for reengineering primary health care services. The clinic is situated within a larger Tshwane metropolitan area, with support structures from a large South African university, the local government and various private organisations.
2. NATIONAL HEALTH INSURANCE
The South African national government proposed a national phased-in strategy to explore and implement a universal coverage model for the South African population in the form of a National Health Insurance (NHI). The Green Paper on NHI emphasises the centrality of primary health care (Department of Health 2011b:23) as the approach to ensure a more equitable health system. Primary Health Care (PHC) services as envisioned in this document will extend beyond the disease-approached model to include preventative health as a central component of community life.
The NHI Green Paper of the Department of Health (2011b:23) emphasize the importance of PHC in developing a model for the NHI: "It has been shown that there is strong support for the inclusion of Primary Health Care services within the benefit package for mandatory insurance. This should also include private primary health care services. This has the potential to reduce the disparities that exist in the distribution of human resources between the public and the private sector."
The Green Paper on NHI (Department of Health 2011b:23) emphasises that the NHI will contribute to an integrated and enhanced National Health Information System. This information system will provide a contribution to the determination of the population's health within South Africa. The Green Paper also proposes that the Health Information System should be an electronically-based platform and should create a linkage between the NHI databases and accredited/contracted service providers. The Green Paper mentions various administrative and technical aspects that have to be considered for the implementation of the NHI. Below follows a summary of these aspects:
■ The implementation should be a phased and systematic approach.
■ Development of a strategy that allows for the strengthening of district health structures to support service delivery within the National Health Insurance.
■ The development and implementation of a comprehensive plan for quality improvement, assurance and compliance for all service providers.
■ Conducting real-life demonstrations and pilots in prioritized health districts.
Figure 1 is a simplified diagram to explain the NHI ICT implementation.
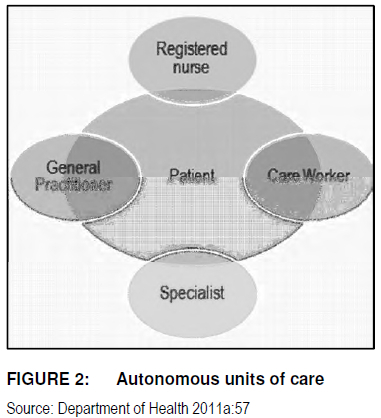
The 2030 strategy on Human Resource for Health in South Africa (Department of Health 2011a:56-57) suggests seeking new opportunities for collaboration amongst health professionals; including a wider representation of the multi-disciplinary team. The recommendation is that patient care models move away from the traditional approach of autonomous units of care as depicted in Figure 2, but rather towards a holistic team approach as seen in Figure 3.
3. DASPOORT CLINIC: RE-ENGINEERING CURRENT SYSTEMS
Daspoort clinic as a service learning site was birthed in 1964 with a group of medical students attached to the University of Pretoria wanting to give back to a local community by practising the learnt skills. Initially patients were seen on Friday evenings and the medical students were supervised by a volunteer general practitioner residing in the area. In 1967 already this clinic moved towards a multi-disciplinary team approach with students from social services, physiotherapy and speech and language pathology also offering services as part of the health team.
In recent years the health team re-affirmed their vision to function as a collaborative care team. In 2013 students from the following health and technology disciplines were involved in service learning at the clinic: medical, nursing, occupational therapy, speech and language pathology, dietetic, oral hygiene, social services, physiotherapy, information technology and technology management. The multi-disciplinary team truly collaborates in managing patients holistically.
Patient consultations categorise individual, clinical and contextual issues and overlapping areas of concern are managed in a team approach. The electronic management system that was implemented as an electronic data capturing system was introduced to the multi-disciplinary team over a period of time. During phase one all patient visits documented by the collaborative team were captured electronically by a data capturer. The data that are currently recorded include: patient diagnosis, ICD code, allocated costs, patient medicine prescribed and referrals with a space for extra notes to be made. The project has made wonderful progress in terms of staff buy-in and meeting before-set goals to move from a paper-based system to a dual model where electronic medical recordkeeping is now part and parcel of the patient consultation.
The entire multi-disciplinary team has slowly been introduced to this system. The last quarter of 2013 all patient records were both manually and electronically recorded. As of 2014 patient consultations from all disciplines will be captured electronically in a similar fashion. More than 7000 patient files have already been created of existing patient paper files. During the last quarter of 2013 over 4000 patients were seen and electronically recorded. This allows for patient profiling such as listing the top diagnosis made at the clinic and what percentage of the patients are controlled or not on current treatment for chronic diseases. A market related costing model is also linked to a diagnosis which enables the clinic to budget accurately and potentially bill patients on a NHI system. The information available to the team opens up endless possibilities to improve health care and strengthen interventions across the multi-disciplinary team.
The current reality for primary health care delivery in South Africa is that often the services offered are uncoordinated, independent and fragmented (Department of Health 2011a:57). The health of the patient is dealt with in micro-pockets of specialities. This may provide for excellent care in certain fields, but the complete health of the patient in terms of his physical, mental and social well-being (World Health Organization 1964:100) is not addressed holistically nor does that guarantee an excellent outcome as the interdependence of these factors often affect the end-result. In 1985 the European region of the World Health Organisation adapted the 1964 definition of health by stating the following: "Health is the extent to which an individual or group is able, on the one hand, to realize aspirations and satisfy needs, and on the other hand, to cope with the environment." (Ivanov & Blue 2009:254).
Starfield (1998:4) describes that in the latter definition health does not become the objective for living, but rather a resource contributing towards it. Starfield depicts Primary Health Care and its determinants of health in the following way, as indicated in Figure 4.
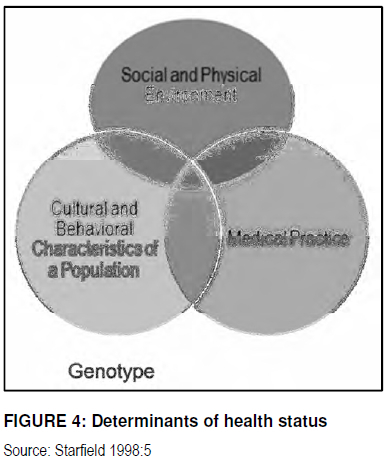
Although the health of a population is indicated by its gene pool (genotype), it is heavily modified by the social and cultural environment and by the nature of health care provided.
The Daspoort Clinic team reflected on the determinants of primary health and the current health and socio-political environment and mapped a strategy for greater collaboration between the medical and social health care systems in the Municipal Ward that they were offering services too. This strategy includes targeted preventative initiatives on the social/environmental sphere of patients with the utilisation of an e-health framework that could develop and strengthen a collaborative team approach to health in its broadest sense with the aim to improve the health of the Daspoort community as situated in Municipal Ward 1, Region 3 of the Tshwane Metropolis.
The project proposed to develop an electronic Integrative Patient Management Model or Health Systems Strengthening Solution (Human Resources and Information Systems) that links all consenting health and social providers on a single patient management system that could simplify and in real-time record and refer patients amongst all the health service participants to assist patients/clients in this municipal ward to attain the latter part of the European region's definition for health: "The extent to which an individual or group is able, on the one hand, to realize aspirations and satisfy needs, and on the other hand, to cope with the environment."
During the first quarter of 2013 all health and social providers in the area were mapped out on a resource list. Everyone were invited to a collaborative care community day to discuss linking of information, sharing of resources and streamlining similar services offered (and often sought out repetitively by the same patients) at various points of care. A number of the NGO's and public organisations signed up to be linked electronically to refer and share patient information seen in an ethical manner cognisant of informed consent and the right to privacy. Many service providers were of the opinion that this could assist to identify 'problem patients' that are over-serviced and often not controlled or taking ownership of their problems. Improved patient care over-all could also be achieved with electronic referrals in real-time and sharing of patient information amongst the team.
4. AN E-HEALTH FRAMEWORK FOR COLLABORATIVE CARE TEAMS
Recent developments in the Information and Communication Technologies (ICT) industries made significant changes on how people are connecting and transferring data. The healthcare industry is slowly converting to the use of such ICT technologies. With the developments in ICT a new healthcare environment was created, namely e-health or eHealth. The development and implementation of an e-health system is essential for future healthcare projects, as mentioned above.
It is important to give a proper definition to what e-heath entails. A number of definitions were found, that could be used to clarify the e-health term. One of the best definitions that where found is:
"E-health is an emerging field in the intersection of medical informatics, public health and business, referring to health services and information delivered or enhanced through the Internet and related technologies. In a broader sense, the term characterized not only a technical development, but also a state-of-mind, a way of thinking, an attitude, and a commitment for networked global thinking, to improve health care locally, regionally, and worldwide by using information and communication technology" (Eysenbach 2002:17).
Another simplified definition is:
"In its simplest form, ehealth is the use of information and communication technologies (ICTs) to facilitate clinical activities, research and education, as well as for monitoring public health." (Jones, Cardos, Hütter, Oliveira, Dos Santos, Lopes & Russomano 2011:334).
Rawabdah (2007:524) argues that e-health has four major categories, namely:
■ medical equipment and supplies: all tangible equipment;
■ health insurance: medical aid members;
■ medication: prescription and over-the-counter medications; and
■ clinical services: online prescriptions.
Rawabdah (2007:524) also states that the essence of e-health is to have reliable transition delivery which is taking place in a fast-changing environment; which includes people, processes, and business infrastructure; focused on ill or healthy citizens.
Rawabdah (2007:524) continues that emerging e-health technologies are oriented to professional networking, the integration of clinical care process management, the provisioning of Web-based health information and patient care, which includes remote monitoring and health care.
During 2012/13 the Daspoort clinic expressed specific needs to assist them in the management of the clinic, their patients and multidisciplinary team, and most of these needs could be addressed with the implementation of an ICT solution.
After a requirement analysis was done the following needs were identified:
a reliable patient management system;
reliable data to be drawn from a database for current health statistics in the community; reliable data for procurement of medicine and medical supplies; accurate dispensing and control of medicine.
4.1 The required ICT technologies
With the implementation of an e-health framework a number of technologies are necessary to assist with the successful implementation of an e-health project. The following technologies were identified:
Handheld devices (e.g. smartphones): the importance of handheld devices are highlighted by Drury (2005:20) and Rawabdah (2007:523), which state that every country wishes to move away from a wired-care environment to a wireless mobile e-health environment, in which several capabilities will evolve, such as hand-held computer, wearable sensors and embedded sensors that can be used for patients who needs routine check-ups and for the provisioning of supplies.
Communication technologies: As described in Drury's 5'C (2005:20) model is the use of communication technology a very important aspect. Developing countries are still faced with the challenge of the availability of reliable and fast internet connections.
Communication technologies are needed to connect the various stakeholders and networked devices; and to transfer the various forms of information between them. Connectivity from remote locations to the internet could take various forms, such as wired (e.g. modem connections) or wireless technologies (e.g. 3G, 4G and LTE).
Server infrastructure: Server infrastructure is needed and should be used as storage areas for patient information repositories. The server will host databases, which is needed to store electronic patient records. It is also important to implement backup infrastructure, needed for safeguarding of the stored information.
Client computers (e.g. laptops and desktop computers): client computers have to be connected to the internet, and will be used to access the information stored on the server infrastructure. Printers and biometric devices could be connected to these computers.
4.2 The implementation of the e-health framework
An e-heath framework for the Daspoort clinic had to be developed and various stakeholders were engaged in the process to develop and implement a workable solution for the clinic. Figure 5 is a visual representation of the implemented solution.
The first two needs for the clinic were: to have a reliable patient management system, and to have access to reliable medical information of the community. These needs could easily be addressed by and e-health system. Below follows a description of the system as it is currently in practise and development.
The initial data capturing during household visits will be done with the use of handheld smartphone device. The handheld device technology and household status assessment questionnaire was developed by a team also linked to the Department of Family Medicine at the University of Pretoria (Bam, Marcus, Hugo & Kinkel 2013:2).
The same technology is available to use at Daspoort clinic as a satellite site for the research conducted from within the Department. In the Community Orientated Primary Care (COPC) approach the community health workers are assigned to households, which they will visit with these handheld devices. As indicated above these devices have a pre-determined set of questions, which should be answered by the households. This will provide information of the current health status of that particular household. All these devices have connectivity to the internet, to enable the devices to transfer data.
Data is also captured within the clinic. All the patient records are being captured and converted into electronic health records. As mentioned earlier over 7000 of the 12 000 patient files were already converted into electronic records.
When a patient reports to the clinic a biometric scan is done to capture a fingerprint of the patient or alternatively his ID or proof of address is used for registration. This is done to identify and verify the patient's identity. Once the electronic patient record is generated it allows the clinical staff to populate the various fields of the e-health record. Once the clinical results are filled the database is updated with the latest information. All the computers within the clinic are connected to a wired network switch and a wireless connection, a 100MB radio link connects the network switch to the University of Pretoria's intranet which then is connected to the internet.
Once the data has been captured by the handheld devices and clinic's computers, it is being transferred over the internet connections to the Health Information Company (HIC). Both sets of data are combined and stored on a centralised Health Information System (HIS) database. By combining all of the captured data of the household; the clinical staff have updated information related to their patients within the service area of the clinic. Additionally the HIS provides the clinic with vital information, such as the current health status of the community.
The Health Information Company (HIC) is connected via the internet to other third party service providers, such a medical aids, pathology laboratories and pharmacies. In future, the HIC could be connected the NHI databases, thus providing the total captured information of a patient to the clinic.
4.3 Implementation strategy
It would be recommended to follow a structured methodology, such as a project management methodology, when embarking on similar projects in the future. Gonzalez & Quesada (2006:146) developed a general framework for the development of an e-health system in Spanish communities. During their study they found six generic phases for system development implementations, such as the one described above. These phases are:
■ the analysis of the current situation and the definitions of the general and specific objectives of the strategy;
■ the collection and analysis of the customer expectations;
■ development of an action plan through cross-evaluation of customer and system needs: utilising techniques such as quality function development (QFD) which included House of Quality (planning matrix), a critical parts matrix and an action plan matrix;
■ cost and strategic analyses: shifting from traditional accounting focus from managing costs to managing the activities that occur within the processes.
■ evaluation and control systems: the implementation of a balanced scorecard, for translating the mission and strategy into actions metrics and indicators which provides the structure for the control and strategic measurement system;
■ the final deployment of the e-health business strategy.
Drury (2005:20) proposed an e-Health framework for developing countries to inform the development of health strategies by utilising available technological resources. The model consists of 5 C's: context, content, connectivity, capacity and community.
Context refers to the role information and communication technologies (ICT) play in enabling the health worker in a context of poverty to provide good quality health care to the patient. ICT should support health workers in providing clinical care, accessing good quality knowledge and patients' medical history and in enabling them to record information.
A major effect of poverty is limited access to care due to cost of travel or treatment. ICT should play a role in providing the health worker access to reliable health information (content) at the place of work.
Wireless connectivity within and between health facilities via hand held devices is proposed to provide an entry-level health information structure. Such wireless infrastructure then makes it possible to build workforce capacity and support community development. The Drury (2005:20-24) electronic health framework was applied to the Daspoort Project as part of the strategic planning to improve health service delivery to the local community.
5. THE DASPOORT CASE STUDY
The WHO's primary health care principles were the foundation for the collaborative care model that is being developed at the Daspoort Clinic. Each of the components above will be addressed in services offered in the future at the Daspoort clinic and in its surrounding community.
5.1 Context
The context of the project is that Daspoort Clinic is an Academic Service Learning site linked to the University of Pretoria. The clinic offers services to an area with multiple socioeconomic problems and a high burden of disease. The clinic is managed as a partnership between the Department of Family Medicine, School of Medicine, University of Pretoria and the Department of Health. The Department of Family Medicine (2007:13) formulated the following vision: "To create a learning environment for pre-graduate health care professionals at the University of Pretoria that builds synergy between service, community resources and scholarly activities through partnerships."
The vision of the service-learning clinic within the context of the re-engineering of primary health care (Department of Health 2011b:23) and the launch of the Health Living Lab which enabled different role-players to collaborate (Hugo, Marcus & Kinkel 2012:25) provided the ideal opportunity for Daspoort Clinic to participate in the regional and national strategies on developing a primary care model that could provide the necessary skills and knowledge to improve health care and access to health care in an equitable fashion.
In order to align with the planned national policy towards a focus on community outreach Daspoort clinic is part of a Community Oriented Primary Care (COPC) programme. This entails Community Health Workers (CHW's) visiting households in a defined geographic area including a nearby informal settlement. At the first visit health related data is gathered during an interview with the family members. The process of data collection is supervised by the Daspoort management team based at the clinic. The data will be analysed after data collection where after interventions to improve the health of the community will be planned. This will be a cyclic continuous process.
5.2 Content
In-time sharing of relevant patient content is an invaluable asset in developing countries where access to health care and patient information sharing amongst health professionals often inhibit optimal health interventions. 'The first issue, therefore, is how to get current knowledge to the health worker in the field in an appropriate format to support them when necessary' (Drury 2005:21).
The management of patient data in the Daspoort community is by means of a Community Oriented Primary Care (COPC) programme. This entails Community Health Workers (CHW's) visiting households in a defined geographic area which is Ward 1, Region 3 for Daspoort clinic including a nearby informal settlement. At the first visit health related data is gathered during an interview with the family members. The data is captured on a hand held devices with a built in interview tool (Mamabolo 2012:6). This household file is then registered against the exact co-ordinates on an online mapping system.
The process of data collection is supervised by the Daspoort management team who is based at the clinic. The patient data collected in the community is then integrated with electronic patient data recorded with the Synaxon system during clinic visits. In 2013 a team of CHW's were trained and household visits with the intent of raising awareness initiated. The CHW's were all assigned to take 200 households early 2014 and handhelds are available to use as soon as the household status assessment that is currently under review is released later 2014.
5.3 Connectivity
Connectivity is essential to the transfer of information between the various stakeholders within the Daspoort community. Drury (2005:22) indicate that WiFi technologies will play an important part in the connectivity of devices within healthcare environments. Connectivity was one of the initial problems encountered at the clinic. Due to the geographical location of the clinic a wired network connection which link the clinic to the University of Pretoria was not possible.
This problem was solved with the installation of a 100MB radio link, which connect the clinic to the IT network infrastructure of the University of Pretoria. All the computers within the clinic connect to a network switch with normal network cables. All the handheld devices which are being used by the Ward Based Outreach Team (WBOT) connect to the HIS databases with GSM data protocols. The implementation of the wireless technologies provide healthcare workers with access to the Internet and update patient information in realtime.
5.4 Capacity
Creating capacity by empowering the Daspoort clinical care team, CHW's and wider health and social network is an on-going process. Lay volunteers were identified by a Faith Based Organisations (FBO) assigned to the regional ward and clinic to assist with the development of a COPC site and a Ward Based Outreach Team (WBOT). The community health workers were trained with an introductory health course which also includes information on the use of the handheld device in data-gathering.
Continuous professional development and support is however a necessity. In future a team consisting of family physicians, general practitioners, allied health including specialist counselling, will be available at the clinic on a weekly basis. Patient information obtained during household visits will be reviewed by the health team and an individual and community diagnosis and strategies decided on. Follow up visits of CHW's to households will be accompanied by the relevant health professional student or organisation member to assist and capacitate the CHW's in providing an optimal treatment response to issues identified. Patients seen at the households will also be electronically referred to the clinic and the service provider network.
5.5 Community
The motivation for the community to extend beyond the health facility (Drury 2005: 23) germinated the creation of a collaborative care model that not only encompasses the multi-disciplinary health professional team, but stretches beyond the clinic border to link through relationship and an electronic referral system NGO's/FBO's and other health and social providers in the Daspoort community. The first community forum meeting was held early 2013 with more than 50 people from over 11 service organisations in the area signing up to join the electronic referral system.
The community network will be strengthened over time to include the nearby secondary referral hospitals. The data will be made available to the relevant health and social providers as patients are seen throughout the continuum of care in the Daspoort community.
Patients will register at each facility and informed consent obtained to allow data gathering and integration at a host facility. The Daspoort Clinic will be the sentinel node within this network, linking patient data collected in the clinic with that obtained in the community and also to other health and social providers up to secondary care level. The utility of technology to strengthen patient care by enabling collaboration amongst a provider network becomes the platform for the Daspoort community model of care.
6. APPLICATION OF THE DASPOORT EXPERIENCE TO FUTURE PRACTICE
Change management (people management) is vital. Firstly the multi-disciplinary team was made up from a large number of stakeholders and management of the buy-in and/ or resistance of stakeholders are key to the success of the project. Secondly clear communication within projects is vital and clear communication paths should be created to provide stakeholders with correct information on the project.
The enthusiasm of the administrative clerk responsible for registering patients when they arrive at the clinic, ensured that thousands of files were created electronically over a short period of time. In-turn this motivated the rest of the personnel to start participating by ensuring the correct information was summarised for after-consultation data capturing.
In resource constraint environments (such as Daspoort) a 'lean start-up approach' in implementation of an eHealth strategy ensured the success. Lean start-up (Ries 2014: Internet) involves the build-measure-learn feedback loop as a core component of its methodology. The first step is to clearly identify the problem or innovation to be solved followed by developing a minimum viable product (MVP) to begin the process of learning as quickly as possible. In other words, clearly identify the needs and the steps to be followed to address the needs in the most cost-effective way; whilst continuously learning on the actions that have been taken and adjusting accordingly.
Small wins motivated the team to go for the next step. A systems development approach assisted project teams to identify the requirements and the various stakeholders needed within the project. Early on identification and mapping of importance of role-players ensured that energy was spent on the people and processes that would provide the highest return.
7. CONCLUSION
The Daspoort case study models an incremental approach for a primary care facility to utilise technology as a tool to meet the needs of the community that it is offering services too. The role of the collaborative care team in achieving the long-term national strategy (Department of Health 2011a:56-58) and also in meeting the needs of the community holistically (Starfield 1998:4) is key in determining the success for anyone planning to implement a technology solution.
An implementation strategy such as the one recommended by Gonzalez & Quesada (2006:146) and the 5 C's framework (Drury 2005:20) were referred to as guiding documents and proofed to be good resources to keep stakeholders informed and track progress in a complex project that needs to be adaptive to clinical, technological and business needs. This assisted the Daspoort team to continually re-focus attention on the agreed objectives.
The project started off with a need to improve service delivery to the community in a manner that meet their needs. More than ever this is still re-iterated by the team. Technology is a tool. Not the final solution, but an invaluable tool in a complex community where one wants to maximise autonomy of patients to achieve the greatest health possible for themselves.
Acknowledgement
The authors would like to thank Synaxon for providing their health technology management solution pro bono for this project.
REFERENCES
BAM N, MARCUS T, HUGO J & KINKEL H-F. 2013. Conceptualizing community oriented primary care (COPC), the Tshwane, South Africa, health post model. African Journal of Primary Health Care and Family Medicine 5(1):1-3. [ Links ]
DEPARTMENT OF FAMILY MEDICINE. 2007. The Daspoort policlinic: an academic learning site for the Pretoria: University of Pretoria. Annual Report: 13. [ Links ]
DEPARTMENT OF HEALTH. 2011a. Human resources for Health South Africa 2030. HRH strategy for the health sector: 2012/13-2016/17 p. 56-58. [Internet: http://www.k4health.org/sites/default/files/RSA_%20HRH_Strategy_draft_Aug2011.pdf; downloaded on 2014-02-10. [ Links ]]
DEPARTMENT OF HEALTH. 2011b. National Health Insurance in South Africa. Policy paper: the re-engineering primary health care system. [Internet: http://www.info.gov.za/view/DownloadFileAction?id=148525; downloaded on 2013-11-01. [ Links ]]
DRURY P. 2005. eHealth: a model for developing countries. eHealth International. pp. 21-26 [Internet: http://www.ehealthinternational.net/; downloaded on 2013-02-01. [ Links ]].
EYSENBACH G. 2002. Issues in evaluating health websites in an Internet-based randomized controlled trial. Journal of Medical Internet Research 4(3):17-20. [ Links ]
GONZÁLEZ ME & QUESADA G. 2006. Conceptual design of an e-health strategy for the Spanish health care system. International Journal of Health Care Quality Assurance 19(2):146-157. [ Links ]
HUGO J, MARCUS T & KINKEL H-F. 2012. Health living laboratory business plan. Budget cycle Oct 2012-Sept 2013. Available on request at the Department of Family Medicine, University of Pretoria. p. 25. [ Links ]
IVANOV LL & BLUE CL. 2009. Public health nursing: leadership, policy & practice. Clifton Park, NY: DelmarCengage Learning. [ Links ]
JONES CR, CARDOSO RB, HÜTTER E, OLIVEIRA HW, DOS SANTOS MA, LOPES MHIL & RUSSOMANO T. 2011. Towards designing for equity: active citizen participation in health. Transforming government. People, Process and Policy 6(4):333-344. [ Links ]
MAMABOLO LFC. 2012. Improvement of the data quality captured through the use of the hand held device for community orientated primary care programme in Tshwane district. Action research report in partial fulfilment of the Certificate in Advanced Health Management, Foundation for Professional Development (FPD); Pretoria. Action Research Report. [ Links ]
RAWABDAH AAA. 2007. An e-health trend plan for the Jordanian health care system: a review. International Journal of Health Care Quality Assurance 20(6):516-531. [ Links ]
RIES E. 2014. The Lean Startup. [Internet: http://theleanstartup.com; downloaded on 2014-09-07. [ Links ]]
STARFIELD B. 1998. Primary care: balancing health needs, services, and technology. Revised edition. New York, NY: Oxford University Press. pp. 3-6. [ Links ]
VIRCHOW R. 1848. In his weekly medical newspaper Die Medizinische Reform, 2. In Henry Ernest Sigerist, Medicine and Human Welfare, (1941): 93. [Internet: http://www.todayinsci.com/V/Virchow_Rudolf/VirchowRudolf-Quotations.htm; accessed on 2014-02-08. [ Links ]]
WORLD HEALTH ORGANISATION. 1964. Preamble to the Constitution of the World Health Organization as adopted by the International Health Conference, New York, 19-22 June, 1946; signed on 22 July 1946 by the representatives of 61 States (Official Records of the World Health Organization, no. 2, p. 100) and entered into force on 7 April 1948. [Internet: http://www.who.int/about/definition/en/print.html; downloaded on 2014-02-10. [ Links ]]
WORLD HEALTH ORGANISATION. 2013. Primary health care. [Internet: http://www.who.int/topics/primary_health_care/en; downloaded on 2013-03-01. [ Links ]]













