Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
Southern African Journal of Critical Care (Online)
versión On-line ISSN 2078-676X
versión impresa ISSN 1562-8264
South. Afr. j. crit. care (Online) vol.40 no.1 Pretoria mar. 2024
http://dx.doi.org/10.7196/SAJCC.2024.v40i1.e1435
RESEARCH
The effect of the SARS-CoV2 pandemic and lockdown on non-Covid ICU admissions: Experience from a South African tertiary hospital
S MurphyI, II; K ZwaneIII, IV; K WilliamsV; S OmarVI, VII
IMB BCh, DCH (SA), FCPaed, Crit Care(SA), MScMed (Bioethics & Health Law); Intensive Care Unit, Chris Hani Baragwanath Academic Hospital, Soweto, Johannesburg, South Africa
IIMB BCh, DCH (SA), FCPaed, Crit Care(SA), MScMed (Bioethics & Health Law); Department of Paediatrics and Child Health, University of the Witwatersrand, Johannesburg, South Africa
IIIMB BCh, DCH (SA); Department of Paediatrics and Child Health, University of the Witwatersrand, Johannesburg, South Africa
IVMB BCh, DCH (SA); Department of Paediatrics and Child Health, Chris Hani Baragwanath Academic Hospital, Soweto, Johannesburg, South Africa
VBHS, MB BCh, DCH (SA), HIVdip (SA); Intensive Care Unit, Chris Hani Baragwanath Academic Hospital, Soweto, Johannesburg, South Africa
VIMB BCh, FCPath (Chem) SA, Crit Care (SA) DA(SA); Intensive Care Unit, Chris Hani Baragwanath Academic Hospital, Soweto, Johannesburg, South Africa
VIIMB BCh, FCPath (Chem) SA, Crit Care (SA) DA(SA); Department of Critical Care Medicine, University of the Witwatersrand, Johannesburg, South Africa
ABSTRACT
BACKGROUND. Future pandemic planning involves analysing past experiences. We compared intensive care unit (ICU) admissions during the SARS-CoV-2 pandemic (2020) with the preceding year.
OBJECTIVES. To assess the SARS-CoV-2 pandemic's effect on ICU admissions in a tertiary hospital, examining differences in patient characteristics, organ support requirements, reason for admission, mortality rates and length of ICU stay.
METHODS. This retrospective cohort study compared ICU patient data at a tertiary hospital during the SARS-CoV-2 pandemic (26 March 2020 to 20 September 2020) with the same period in 2019.
RESULTS. Patient admissions (p=0.39) and severity of illness (p=0.27 adults; p=0.92 paediatrics) showed no differences across the study period. Similarly, no differences were observed for underlying chronic conditions between the two years. Adult trauma admissions significantly declined, specifically those related to road traffic accidents (RR 0.63). Admissions for acute infectious conditions, including respiratory infections, sepsis, urosepsis, septic arthritis and gastroenteritis significantly declined in both adults (RR 0.50) and paediatric admissions (RR 0.25). During the lockdown period, the length of stay (LOS) decreased for adults, but mortality rates remained unchanged across the study period. The paediatric mortality rate decreased during the lockdown period (p=0.004).
CONCLUSION. There was no reduction in SARS-CoV-2-negative ICU admissions during the 2020 lockdown period compared with the preceding year, likely due to chronic resource limitations. We found a decrease in acute trauma and acute infectious illness admissions, while acute surgical emergency admissions increased. These findings suggest that lockdown orders may have affected admission patterns, aiding in future pandemic planning.
The World Health Organization (WHO) has recently launched a new initiative, Preparedness and Resilience for Emerging Threats (PRET), to improve pandemic preparedness and response strategies within member countries.[1] It is therefore prudent to locally reflect on what the effect of the lockdown and subsequent restructuring of healthcare services had on our non-COVID critically ill patients.
The pandemic highlighted many deficiencies within our healthcare system, particularly its inequities and chronic overburdening. It has emphasised the prevailing issue of inadequate resources and persistent shortages of ICU beds, which have become the norm.[2] The focus of the government strategy was on preparing for and expanding capacity through the implementation of 'lockdown'/stay-at-home orders, coupled with restrictions on alcohol sales and travel. These measures resulted in reduced hospital emergency department visits and admissions among adult patients presenting with injuries due to trauma.[3-9] This allowed hospital beds and human resources to be redirected to those presenting with severe illness due to SARS-CoV-2. However, the lockdown brought about some undesirable consequences: access to healthcare became difficult for some,[10] and there was reluctance among others to visit hospitals owing to the potential risk of virus transmission.
At Chris Hani Baragwanath Academic Hospital, preparation for the anticipated surge in admitted SARS-CoV-2 patients included the creation of separate areas designated for SARS-CoV-2-positive and negative patients within the hospital across all disciplines. The 26-bedded Main intensive care unit (ICU) was reserved for admissions of patients who tested negative for SARS-CoV-2, including adult and paediatric medical, surgical and trauma patients. The ICU established a mobile polymerase chain reaction (PCR) laboratory by non-laboratory healthcare workers, which proved to be a rapid (150 minutes), accurate and clinically effective solution for allocating patients to the SARS-CoV2 positive and negative areas.[11] A separate ICU, with a capacity to accommodate 24 patients, was created for SARS-CoV-2 patients. The new COVID ICU was staffed by existing ICU nursing and medical staff, as well as newly employed staff and individuals seconded from other hospital areas. Nurse-to-patient ratios of 1:1 was maintained, and capacity was dependent on number of nurses available each day.
In many high-income countries, the reported mortality and length of stay among SARS-CoV-2-negative critically ill patients admitted to ICU remained the same or improved when compared with a pre-pandemic period, whereas in middle-income countries, higher mortality was observed.[12-14] Locally, pre and post-pandemic ICU mortality among SARS-CoV-2-negative admissions in one province was unchanged, which was attributed to critical care resiliency and more longitudinal experience in resource-limited environments such as South Africa (SA).[15] We sought to investigate the effect of the lockdown on the number of SARS-CoV-2-negative admissions at our multidisciplinary ICU during the pandemic, compared with the pre-pandemic period.
Methods
Study setting
Chris Hani Baragwanath Academic Hospital is a tertiary academic hospital in Soweto, Johannesburg, South Africa, with a total bed capacity of ~3 500. It serves the Soweto community and broader Johannesburg areas.
Study design
This was a descriptive retrospective cohort study that investigated the impact of the SARS-CoV2 pandemic on the number, type of admission and outcomes of patients who tested negative for SARS-CoV-2 and were accommodated in the Main ICU between 26 March 2020 (the beginning of the lockdown period) to 20 September 2020 (when the country returned to alert level 1 and most normal activity resumed). This was compared with the same period in the preceding year.
Primary objective
To compare the total number of ICU admissions between the two study periods (2019 and 2020)
Secondary objectives
To compare the general patient characteristics between the two periods, including age; sex and illness severity, examined using the Simplified Acute Physiology Score (SAPS) for adult admissions and Paediatric Index of Mortality Score (PIM 3) for paediatric admissions; the presence of comorbidities (assessed using the Charlston comorbidity index), and HIV status.
To also compare organ support requirements (respiratory, cardiovascular and renal replacement therapy) upon admission to the ICU during the two time periods. Furthermore, we aimed to compare the proportion of patients admitted during the two periods across diagnostic categories (Trauma, Medical, Surgical and Obstetric), including sub-groups within each category. Finally, we sought to compare the length of stay (LOS) and mortality outcomes during the two periods.
Data collection
The ICU files of all patients admitted to the multidisciplinary Main ICU at Chris Hani Baragwanath Academic Hospital during the two time periods were retrieved and reviewed. The data were retrospectively collected into an electronic data collection tool (REDCap).[16] Patient information was collected for all the adult and paediatric ICU patients (Medical, Surgical and Trauma) admitted to the Main ICU (excluding high-care admissions). Demographic information, including age, sex, HIV status, presence of comorbidities (Charleston co-morbidity Index for adult patients), and Illness severity (SAPS II for adult patients and PIM 3 for paediatric patients). Diagnoses at admission were documented and classified into diagnostic categories and sub-groups. Organ support requirements upon admission (ventilation, pressors and renal replacement therapy) were also recorded, along with ICU LOS and patient outcome (death or survival during ICU stay) for each case.
Ethical clearance
This research project was approved (ref. no. M201118) by the Human Research Ethics Committee (HREC) of the University of the Witwatersrand. Consent from participants to use their data was waived.
Statistical analysis
Descriptive statistics were used to report the data. Categorical variables were described using frequencies and percentages. Continuous variables were described using medians and interquartile ranges (IQR) where the data were not normally distributed and means and standard deviations (SD) where the data were normally distributed. Comparisons between groups were performed using the Mann-Whitney-U test for categorical variables and were described using odds ratios with 95% confidence intervals (CI). Calculations were performed using Statistica version 13.3 (StatSoft, USA). To detect a 5% reduction in admission rates between the two periods, starting with a proportion of 0.516 (2019), a sample size of 783 was required for a statistically significant change at p<0.05 and 80% power).
Results
Primary outcome
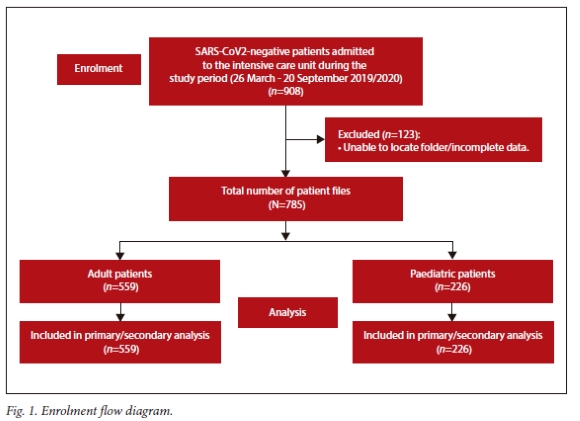
In total, 908 patients were admitted to the ICU (Adult, Paediatric and Trauma) during the two periods (26 March to 20 September 2019 and 2020). Of those, 123 patients were excluded due to the inability to locate complete patient folders and the information required to complete the data sheet (Fig. 1). There were no differences in admission numbers between the two periods (p=0.39) (Table 1).
Secondary outcomes
No significant differences were noted between the 2019 and 2020 patient groups concerning sex, presence of comorbidities, HIV status and illness severity scores. The median age of paediatric admissions was significantly higher during the lockdown period (Table 2).
Organ support requirements
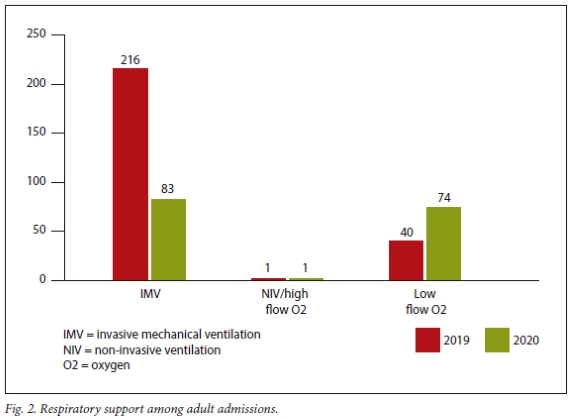
Respiratory
Among adults, the relative risk of receiving non-invasive respiratory support during 2019 was lower than in 2020 (Relative Risk (RR) 0.55, 95% CI 0.39 - 0.76). Among paediatric patients, the relative risk of receiving high-frequency oscillatory ventilation (HFOV) in 2019 was not different than in 2020 (RR 2.69, 95% CI 0.99 - 7.40) (Fig. 2).
Cardiovascular
Among adult admissions, there was a greater risk of cardiovascular dysfunction (the requirement for inotropes or vasopressors) among patients admitted in 2019 compared with those admitted in 2020 (RR .35, 95% CI 1.04 - 1.74), whereas there was no significant difference among paediatric admissions (x2 0.47, p=0.49).
Renal
For adult admissions, the relative risk of acute kidney injury (AKI) among patients in 2019 was 1.6 times greater than that in patients admitted in 2020 (95% CI 1.19 - 2.15). However, there was no significant difference in the risk of AKI for the same period among paediatric admissions (x2 0.03, p=0.86).
Admission diagnoses
Adult ICU admissions
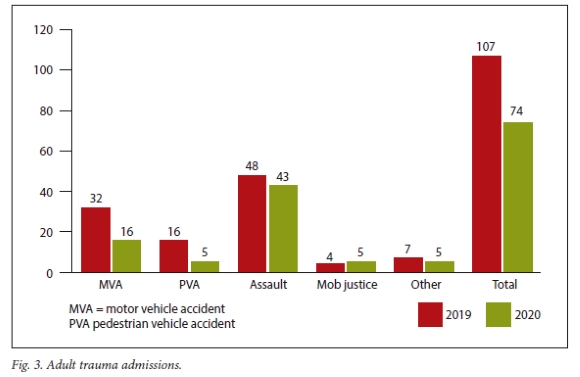
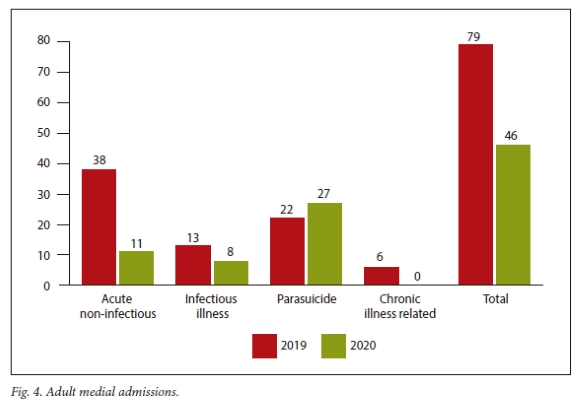
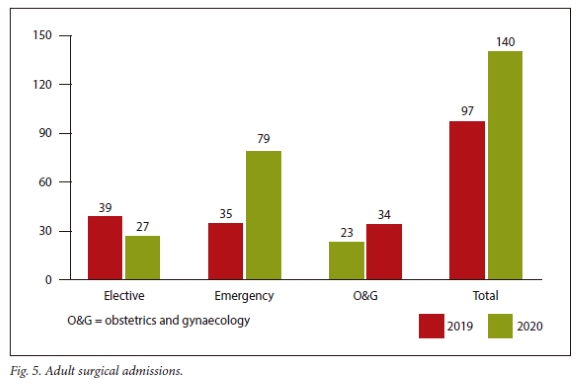
In 2020, during the lockdown period, there was a decrease in the total number of admitted patients who had sustained traumatic injuries. Specifically, there was a significant decrease in road traffic accident admissions compared with 2019, with an RR of 0.63 (95% CI 0.42 - 0.94). Among medical admissions, there was a significant decrease in acute medical admissions not related to infectious disease in 2020 compared with 2019 (RR 0.50; 95% CI 0.30 - 0.87). Emergency surgical admissions significantly increased in 2020 compared with 2019 (RR 1.56 95% CI 1.18 - 2.08) (Figs. 3-5).
Paediatric admissions
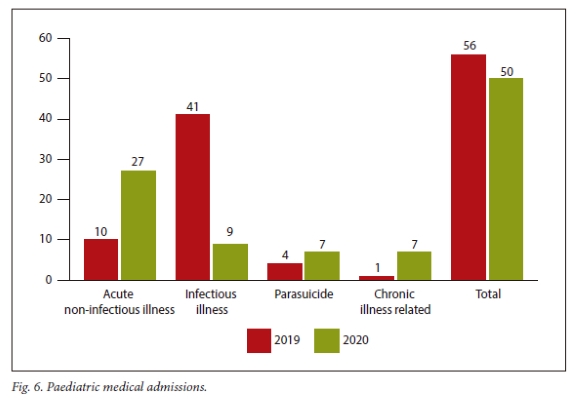
There was a significant decrease in admissions related to acute infectious illness in 2020 compared with 2019 (RR 0.25 95% CI 0.15 -0.40). There were no significant differences in paediatric surgical and trauma admissions between 2019 and 2020 (Fig. 6).
Length of stay and ICU mortality
The overall length of ICU stay was significantly reduced in 2020 compared with 2019 (Table 3). This was statistically significant in the adult admission group, although the same trend was observed in the paediatric sub-group. The risk of death among paediatric patients admitted during 2019 was significantly higher than in 2020 (RR 6.3; 95% CI 1.3 - 30.2). However, overall ICU mortality was not significantly different between the two time periods.
Discussion
The number of patients admitted to the ICU
It was anticipated that there would be a decrease in the total number of ICU admissions among SARS-CoV-2-negative critically ill patients , as demonstrated in previous studies.[17-23] We also presumed that the secondary effects of lockdown, such as reduced public transport, movement restrictions and concerns about contracting the virus from healthcare centres, would deter individuals from accessing healthcare services, thereby resulting in decreased hospital and ICU admissions.
However, when comparing the total number of ICU admissions between the two periods (2019 pre-lockdown and 2020 during lockdown), there was no statistically significant difference in patient admission numbers (p=0.39). This is likely because this ICU experiences chronic resource limitations, where the demand for beds exceeds availability daily. Chronic resource limitation is defined as the need to refuse patients' ICU admission on most days. As highlighted in a systematic review from 2015, resource-limited facilities typically have an average range of ICU beds available between 0.1 - 1.7 per 100 000 patients, in contrast to 33.6 beds in developed countries.[24] Consequently, while there might have been a decline in the number of patients requiring ICU admission, the admission figures remained unchanged because the demand for ICU beds consistently exceeds bed availability in this ICU. Furthermore, those adults and children who were highly ill continued to seek medical attention during the lockdown period.
Types of patients admitted to the ICU
Other SA trauma centres have already demonstrated reductions in absolute numbers of trauma admissions by 25 - 59% during the SA lockdown,[5-8] declines in road traffic accidents by as much as 40%[8] as well as reductions in the severity of trauma admissions[8] compared with the same period pre-lockdown. There was a significant decline in adult trauma admissions to our ICU, specifically related to road traffic accidents (RR 0.63; 95% CI 0.42 - 0.94). There was no significant increase in gender-based violence or self-inflicted harm. Among paediatric trauma admissions, there was no difference in the number of trauma and emergency surgical admissions over the two distinct periods, which is in keeping with other published data concerning paediatric hospital and ICU admissions during the lockdown period.[22,25,26]
The number of emergency surgical admissions significantly increased during the lockdown period compared with pre-pandemic. This could be attributed to delays in seeking medical assistance, stemming from fear of visiting healthcare institutions or encountering challenges in accessing healthcare owing to travel restrictions and curfews that were enforced. Among medical admissions, there were notable reductions in admissions for acute infectious conditions, including respiratory infections, sepsis, urosepsis, septic arthritis and gastroenteritis, in both adult and paediatric admissions. In a population-based observational study on the indirect effects of the SARS-CoV-2 pandemic on childhood infection in England, significant reductions in hospital admissions for respiratory, severe invasive and vaccine-preventable diseases were observed across all demographic sub-groups of children, including those with pre-existing comorbidities during the lockdown period.[27] The authors concluded that the public health measures to reduce SARS-CoV-2 transmission also effectively reduced the transmission of other infectious diseases. The decrease in ICU admission numbers for acute infectious conditions in our ICU may stem from the same effect and has also been demonstrated in other institutions.[23] Specifically, the closure of schools and day-care centres, social distancing, mask-wearing, prohibition of large social gatherings and restrictions of movement, as well as general measures such as handwashing and self-isolation during periods of illness may all have resulted in these reductions of acute infectious diseases in both adult and paediatric patients.
The number of patients admitted to the ICU after a suicide attempt increased during the lockdown period compared with the previous year, however these differences were not statistically significant, as have been demonstrated in other parts of the world.[28] Locally, increases in common mental disorders, such as anxiety and depression and psychological distress have been found in a cohort of perinatal women as well as people living with HIV in SA during lockdown.[29,30]
Patient severity of illness and organ support requirements
Contrary to expectation, this study found no evidence supporting the assumption that the patients admitted during the lockdown period would be sicker due to delays in seeking medical assistance and that adult patients admitted to ICU would have multiple chronic conditions. This is in keeping with findings in other parts of the world.[23,31] There was no difference in the severity of illness scores among adult and paediatric ICU admissions, nor was there an increase in the number of patients admitted with chronic underlying medical conditions.
Regarding respiratory support requirements, more adults received non-invasive support during the lockdown period compared with the pre-lockdown period. We found significantly increased use of non-invasive respiratory in the adult ICU admissions, predominantly humidified high-flow nasal oxygen. The increased use of humidified high-flow nasal oxygen (HHFNO) could be attributed to several factors. First, the pandemic led to greater availability of HFFNO in the ICU. Second, new research showing the benefits of HFFNO, previously unavailable, emerged during this time. This approach has been shown to prevent or decrease the number of patients requiring invasive mechanical ventilation due to hypoxic respiratory failure, regardless of their COVID status.[32]
This same trend was not observed among paediatric admissions, possibly because high-flow oxygen is routinely used in the paediatric wards and high-care areas at this hospital and failure of a trial of HFFNO usually results in intubation and ventilation and subsequent ICU admission.
Cardiovascular support during the lockdown period was significantly reduced compared with pre-lockdown (relative risk 1.35%), as was the need for renal replacement therapy (RRT) among adult admissions. This trend could be explained by the decrease in admissions for acute infectious conditions, as described above, leading to a subsequent reduction in the incidence of sepsis and septic shock.
Patient outcomes
The overall length of ICU stay decreased during the lockdown period but this was only significant in adult admissions. These findings are similar to those reported elsewhere, and could be attributed to patients being less severely ill and having a lower burden of acute infectious illnesses, despite there being no difference in mortality and illness severity scores between the two groups.[17]
Paediatric mortality was reduced during the lockdown period, which may again reflect the lower burden of acute infectious illness seen during the lockdown period and the increased median age of patients admitted. This combination of older patients and fewer acute infectious illnesses would be expected to result in better ICU outcomes.
Limitations
This study had a few limitations. Filing and storing of patient records remains a significant challenge, in the absence of an electronic patient record base. This was worsened during the pandemic due to shortages of ward clerks during this period. Although both the Main and SARS-CoV-2 ICUs were functioning at full capacity during these periods, bed availability depended on the ability to maintain a nurse-to-patient ratio of 1:1. Therefore, the number of functional beds varied depending on staffing capability. We do not have accurate information on how the capacity change varied from day to day for these periods.
Conclusions
We did not find a reduction in SARS-CoV-2-negative ICU admissions during the 2020 lockdown period compared with the preceding year. This is likely due to the chronic resource limitation, which this unit experiences consistently. We did however find reductions in acute trauma admissions and acute infectious illness, while acute surgical emergency admissions increased. We postulate that these findings may be an effect of the lockdown orders. These findings help in planning for future pandemic preparedness.
Declaration. None.
Acknowledgements. The authors acknowledge all the medical establishment staff who tirelessly worked during the SARS-CoV-2 pandemic at Chris Hani Baragwanath Academic Hospital.
Author contributions. Authors contributed as follows to the conception and design of the work; acquisition, analysis and interpretation of data; drafting the final manuscript and revising it critically: SM 40%, KZ 35%, SO 20%, KW 5%.
Funding. No funding was received for this study. All costs were covered by the investigators in their personal capacities.
Conflicts of interest. None.
References
1. Black C. WHO launches new initiative to improve pandemic preparedness. 2023 Apr 26. https://reliefweb.int/report/world/who-launches-new-initiative-improve-pandemic-preparedness (accessed 21 June 2023). [ Links ]
2. Abdool Karim SS, Kelemu S, Baxter C. COVID-19 in Africa: Catalyzing change for sustainable development. PLOS Med 2021 Nov 29;18(11): e1003869. https://doi.org/10.1371/journal.pmed.1003869 [ Links ]
3. Hendrikse C, Parak M, Van Hoving DJ. A descriptive analysis of the effect of the national COVID-19 lockdown on the workload and case mix of patients presenting to a district-level emergency centre in Cape Town, South Africa. S Afr Med J 2020 Oct 12;110(11):1113. http://dx.doi.org/10.7196/samj.2020.v110i11.15028 [ Links ]
4. Effect of the COVID-19 lockdown regulations on the severe trauma burden in an urban trauma centre in Johannesburg, South Africa. J Surg 2022 Dec 6;7(16). https://www.gavinpublishers.com/article/view/effect-of-the-covid-19-lockdown-regulations-on-the-severe-trauma-burden-in-an-urban-trauma-centre-in-johannesburg-south-africa (accessed 25 May 2023). [ Links ]
5. Mahoney SH, Steyn E, Lategan H. Informing future policy for trauma prevention: The effect of the COVID-19 "National state of disaster lockdown' on the trauma burden of a tertiary trauma centre in the Western Cape of South Africa. Afr J Emerg Med 2021 Sep;11(3):361-365. https://doi.org/10.1016/j.afjem.2021.06.002 [ Links ]
6. Navsaria PH, Nicol AJ, Parry CDH, Matzopoulos R, Maqungo S, Gaudin R. The effect of lockdown on intentional and nonintentional injury during the COVID-19 pandemic in Cape Town, South Africa: A preliminary report. S Afr Med J 2020 Dec 14;111(2):110. https://hdl.handle.net/10520/ejc-m_samj-v111-n2-a8 [ Links ]
7. Chu KM, Marco J, Owolabi EO, et al. Trauma trends during COVID-19 alcohol prohibition at a South African regional hospital. Drug Alcohol Rev 2022 Jan;41(1):13-19. https://doi.org/10.1111/dar.13310 [ Links ]
8. Venter A, Lewis CM, Saffy P, Chadinha LP. Locked down: Impact of COVID-19 restrictions on trauma presentations to the emergency department. S Afr Med J 2020 Dec 4;111(1):52. https://hdl.handle.net/10520/ejc-m_samj-v111-n1-a15 [ Links ]
9. Akuaake LM, Hendrikse C, Spittal G, Evans K, van Hoving DJ. Cross-sectional study of paediatric case mix presenting to an emergency centre in Cape Town, South Africa, during COVID-19 . BMJ Paediatr Open 2020 Sep;4(1):e000801. https://doi.org/10.1136/bmjpo-2020-000801 [ Links ]
10. Elmi N, Smit L, Wessels T, Zunza M, Rabie H. COVID-19 lockdown effect on healthcare utilisation and in-hospital mortality in children under 5 years in Cape Town, South Africa: a cross-sectional study. J Trop Pediatr 2023 Oct 5;69(6):fmad035. https://doi.org/10.1093/tropej/fmad035 [ Links ]
11. Omar S, Brown JM, Mathivha RL, Bahemia I, Nabeemeeah F, Martinson N. The impact of a mobile COVID-19 polymerase chain reaction laboratory at a large tertiary hospital during the first wave of the pandemic: A retrospective analysis. S Afr Med J 2021 Oct; 111(10);957-960. https://hdl.handle.net/10520/ejc-m_samj_v111_n10_a13 [ Links ]
12. McLarty J, Litton E, Beane A, et al, Linking of Global Intensive Care (LOGIC) Collaboration. Non-COVID-19 intensive care admissions during the pandemic: a multinational registry-based study. Thorax 2023 May 24:thorax-2022-219592. https://doi.org/10.1136/thorax-2022-219592 [ Links ]
13. Bologheanu R, Maleczek M, Laxar D, Kimberger O. Outcomes of non-COVID-19 critically ill patients during the COVID-19 pandemic: A retrospective propensity score-matched analysis. Wien Klin Wochenschr 2021 Sep;133(17-18):942-950. https://doi.org/10.1007/s00508-021-01857-4 [ Links ]
14. Park BD, Kannappan A, Rizzo AN, et al. Relationship between a state-directed lockdown on non-COVID-19 -related ICU admissions and mortality in a multicenter Colorado Healthcare System. Crit Care Explor 2022 Dec 5;4(12):e0791. https://doi.org/10.1097/CCE.0000000000000791 [ Links ]
15. Anesi GL, Savarimuthu MD, Invernizzi J, Hyman R, Ramkillawan A, Eddey C, Wise RD, Smith MTD. ICU mortality across pre-pandemic and pandemic cohorts in a resource limited setting: a Critical care resiliency analysis from SA. CHEST Crit Care June 2023;1(1):1000005. https://doi.org/10.1016/j.chstcc.2023.100005 [ Links ]
16. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)?A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009 Apr;42(2):377-381. https://doi.org/10.1016/j.jbi.2008.08.010 [ Links ]
17. Bagshaw SM, Zuege DJ, Stelfox HT, et al. Association between pandemic coronavirus disease 2019 public health measures and reduction in critical care utilisation across ICUs in Alberta, Canada. Crit Care Med 2022 Mar;50(3):353-362. https://api.semanticscholar.org/CorpusID:237453275 [ Links ]
18. Santi L, Golinelli D, Tampieri A, Farina G, Greco M, Rosa S, et al. Non-COVID-19 patients in times of pandemic: Emergency department visits, hospitalisations and cause-specific mortality in Northern Italy. Manzoli L, editor. PLOS ONE 2021 Mar 22;16(3):e0248995. https://doi.org/10.1371/journal.pone.0248995 [ Links ]
19. Bodilsen J, Nielsen PB, S0gaard M, et al. Hospital admission and mortality rates for non-covid diseases in Denmark during covid-19 pandemic: Nationwide population-based cohort study. BMJ 2021 May 24;373. https://doi.org/10.1136/bmj.n1135 [ Links ]
20. Waseem S, Nayar SK, Hull P, et al. The global burden of trauma during the COVID-19 pandemic: A scoping review. J Clin Orthop Trauma 2021 Jan;12(1):200-207. https://doi.org/10.1016/j.jcot.2020.11.005 [ Links ]
21. Jacob S, Mwagiru D, Thakur I, Moghadam A, Oh T, Hsu J. Impact of societal restrictions and lockdown on trauma admissions during the COVID-19 pandemic: A single-centre cross-sectional observational study. ANZ J Surg 2020 Nov;90(11):2227-2231. https://doi.org/10.1111/ans.16307 [ Links ]
22. Erdede O, Sarı E, Uygur Külcü N, Sezer Yamanel RG. The impact of COVID-19 lockdown on pediatric hospital admissions in Turkey. J Pediatr Infect Dis 2022 Sep;17(05):227-233. [ Links ]
23. Cassell K, Zipfel CM, Bansal S, Weinberger DM. Trends in non-COVID-19 hospitalisations prior to and during the COVID-19 pandemic period, United States, 2017-2021. Nat Commun 2022 Oct 8;13(1):5930. https://doi.org/10.1038/s41467-022-33686-y [ Links ]
24. Tumukunde J, Sendagire C, Ttendo SS. Development of intensive care in low-resource regions. Curr Anesthesiol Rep 2019 Mar;9(1):15-17. https://doi.org/10.1007/s40140-019-00307-2 [ Links ]
25. Gillory L, Cairo S, Megison S, Vinson L, Chung DH, Ryan ML. Effect of quarantine and reopening measures on pediatric trauma admissions during the 2019 SARS-CoV2 virus pandemic. J Am Coll Surg 2022 Apr;234(4):685-690. [ Links ]
26. McIntosh A, Bachmann M, Siedner MJ, Gareta D, Seeley J, Herbst K. Effect of COVID-19 lockdown on hospital admissions and mortality in rural KwaZulu-Natal, South Africa: Interrupted time series analysis. BMJ Open 2021 Mar;11(3):e047961. https://doi.org/10.1136/bmjopen-2020-047961 [ Links ]
27. Kadambari S, Goldacre R, Morris E, Goldacre MJ, Pollard AJ. Indirect effects of the covid-19 pandemic on childhood infection in England: Population based observational study. BMJ 2022 Jan 12; e067519. https://doi.org/10.1136/bmj-2021-067519 [ Links ]
28. Eden CM, Zhu R, Khedr S, Khariton K. Effect of the coronavirus disease 2019 pandemic on suicide-related trauma burden at a level 1 trauma center. J Emerg Trauma Shock 2022;15(2):88-92. [ Links ]
29. Abrahams Z, Boisits S, Schneider M, Prince M, Lund C. The relationship between common mental disorders (CMDs), food insecurity and domestic violence in pregnant women during the COVID-19 lockdown in Cape Town, South Africa. Soc Psychiatry Psychiatr Epidemiol 2022 Jan;57(1):37-46. https://doi.org/10.1007/s00127-021-02140-7 [ Links ]
30. Campbell LS, Masquillier C, Knight L, et al. Stay-at-home: The impact of the COVID-19 lockdown on household functioning and ART adherence for people living with HIV in three sub-districts of Cape Town, South Africa. AIDS Behav 2022 Jun;26(6):1905-1922. https://doi.org/10.1007/s10461-021-03541-0 [ Links ]
31. Rajput K, Sud A, Rees M, Rutka O. Epidemiology of trauma presentations to a major trauma centre in the Northwest of England during the COVID-19 level 4 lockdown. Eur J Trauma Emerg Surg 2021 Jun;47(3):631-636. https://doi.org/10.1007/s00068-020-01507-w [ Links ]
32. Calligaro GL, Lalla U, Audley G, et al. The utility of high-flow nasal oxygen for severe COVID-19 pneumonia in a resource-constrained setting: A multi-centre prospective observational study. E Clin Med 2020 Nov;28:100570. https://doi.org/10.1016/j.eclinm.2020.100570 [ Links ]
 Correspondence:
Correspondence:
S Murphy
susan.murphy@wits.ac.za
Accepted 5 March 2024
Contribution of the study
The study highlights the chronic shortage of critical care resources in South Africa and aids with future pandemic preparedness and planning in a resource limited setting.














